Bonding ceramic restorations
Porcelain and glass ceramics need to be bonded to teeth for the reinforcement of restorations: according to studies, the best results are achieved by pretreating and etching the ceramic surface with hydrofluoric acid, then applying a silane coupling agent or a ceramic primer, and luting with a light- or dual-cured adhesive cement, depending on the restoration thickness. Zirconia may be cemented after gentle roughening by airborne abrasion (grit-blasting) using an adhesive resin composite cement. In addition, tribochemical silica coating combined with silane application is an alternative that might provide enhanced adhesion. The best durable bonding to zirconia is achieved by applying a dual-cured adhesive resin composite cement that contains phosphate ester groups. Among the clinically relevant parameters involved in choosing an adhesive cement system to bond ceramic restorations to the dental hard tissues, the aesthetic properties, colour stability, ease of handling, and appropriate working times of the cement are to be considered.
Key points | |
|---|---|
· |
This article presents the recommended surface pretreatments for the main groups of dental ceramics (porcelain, glass ceramic, and zirconia) for bonding to the dental hard tissues. Clinically relevant aspects related to the bonding of dental ceramics, as well as the reasons for bonding, are also addressed and explained. |
Treatment decisions are based on prevailing clinical conditions, recommendations, and the patient preferences, which affect the design of the tooth preparation, the choice of restoration, and cementation materials. The clinical success of all-ceramic dental restorations, in particular porcelain or glass ceramics, depends on adhesion, i.e., durable bonding between dental materials and tooth substance and thereby the obtained adhesive strength (bond strength). In order to achieve durable and optimal bonding, it is preferable that the preparation (or at least the preparation margins) lies in the enamel. Optimal bonding, is, however, not always possible. In clinical situations, of large destructions of teeth and deep subgingival margins, there is usually little or no enamel left; thus there is considerable risk of contamination of the interfaces to be bonded, and the procedure might become unreliable. The use of a rubber dam may be helpful, although it is not always possible. If an all-ceramic restoration is to be fabricated in a clinical situation where bonding with resin composite cement is suboptimal, the choice could fall onto a zirconia restoration bonded with resin-modified glass ionomer cement, provided that macro- and micromechanical retention are available by means of tooth preparation.
Bonding to ceramic materials
Tooth tissues do not possess any natural affinity to dental ceramics. This is why proper pretreatment and adhesive resin composite cements are vital when bonding ceramic materials to the tooth. Adhesive cementation is understood to be predominantly based on micromechanical and chemical retention. This promotes the preservation of tooth substance. For all-ceramic restorations made of porcelain or glass ceramic, adhesive cementation (based on, e.g., reactive organophosphate monomers) is essential to reinforce the ceramic material, thus allowing resistance to the forces to which they are exposed (1-3).
Before cementation of an indirect restoration, the tooth structures and the indirect restoration need a pretreatment. In general, a pretreatment in dentistry is defined as one or a series of steps such as etching, roughening, cleaning, removal of any debris, so that an adhesive or adhesion promoter can be applied for durable bonding (4,5). The literature describes several methods of surface pretreatment and modifications. These methods can alter the surface properties of the ceramics - chemically, physically, or both - and enable durable bonding between the adhesive cement and the pretreated ceramic surfaces (6,7).
Depending on the type of ceramic, adhesion to its surface can be significantly increased by one of three surface pretreatments: (i) chemical pretreatment with hydrofluoric acid (HF) etching (or an alternative etchant), (ii) physical pretreatment such as grit-blasting (air-borne abrasion) with alumina powder to roughen the surface, and (iii) grit-blasting with silica-coated alumina particles, a method that leaves a silica layer to be subsequently silanised before an adhesive resin composite cement is applied.
Acid etching is typically performed with 5-10 % gel-like HF, which dissolves the glass matrix of porcelains or glass ceramics (8) and creates a micro-porous surface. These porosities enhance micro-mechanical interlocking for durable bonding. Despite the proven positive effect of HF etching on the adhesion to porcelains and glass ceramics, alternative surface pretreatment methods have been proposed to replace HF etching, primarily due to its high toxicity. With such alternative pretreatments, the surface of porcelains and glass ceramics is: (i) etched and chemically activated with a self-etching ceramic primer that contains tetrabutylammonium fluoride (TBAF), or (ii) etched with acidulated phosphate fluoride (APF), or (iii) ammonium hydrogen difluoride (NH4HF2) prior to cementation (9). Currently, using HF is recommended.
The physical pretreatment involves grit-blasting (also called air-borne particle abrasion or sandblasting) with alumina (Al2O3) powder. The physical surface pretreatment optimises adhesion by (i) generating a clean surface with high surface free energy and low surface tension and by (ii) creating a roughened surface for retention, thereby making the surface more reactive for bond formation. A specific form of grit-blasting is tribochemical silica-coating, which utilises silica-coated alumina particles for creating a freshly formed silica layer onto the surface of the indirect restoration. Such silica-coating needs to be followed by a mandatory silane coupling agent (silane) application (10,11). A wide range of intra- and extra-oral indications for tribochemical silica-coating exist, and this pretreatment has been suggested for zirconia bonding (9).
After acid etching, the porcelain, glass ceramic, or silica-coated zirconia surface needs to be silanised. Silane-based adhesion promotion chemistry is very complex. Silane molecules are characterised by direct Si-C bonds. The silane coupling agents are so-called trialkoxysilanes with methoxy groups, -OCH3, and an organofunctional moiety at the other end of the molecule, separated by a linker part, -(CH2)n-. The generally used silane monomer in dental products is 3-methacryloxypropyltrimethoxysilane (MPS). Silanes are not usually called adhesives but rather adhesion promoters (6). In essence, first the hydrophilic silane coupling agent wets the siliceous substrate surface and forms a 3D hydrophobic siloxane film, which strongly chemically bonds to the silica-rich surface. Then exposed unreacted C = C bonds of silane react with the resin composite cement (12). The substrate surface for silane-based adhesion needs to be siliceous: silica, silicates, or glass is mandatory (10). The silane coupling agent molecules are bifunctional synthetic hybrid inorganic-organic molecules. When silane is deposited on an inorganic surface, silanol oligomers react with each other, forming siloxane bonds, -Si-O-Si, which interact with the hydroxyl groups (-OH) on the surface of the silica-rich restoration (Fig. 1). Silanisation allows the formation of covalent C-C bonds between the silanised ceramic surface and the adhesive cement (6,12). In dentistry, clinically used silane coupling agents are pre-activated: the silane concentration is usually ca. 2 vol. %, dissolved in ethanol with a few vol. % of water, and pH set at 4-5 for hydrolysis i.e., activation of the silane molecules (6,12,13).
The recommended pretreatments for the current ceramics, based on the available evidence, are described in detail below and summarised in Table 1. The preferable choice of adhesive cement system is presented in Table 2.
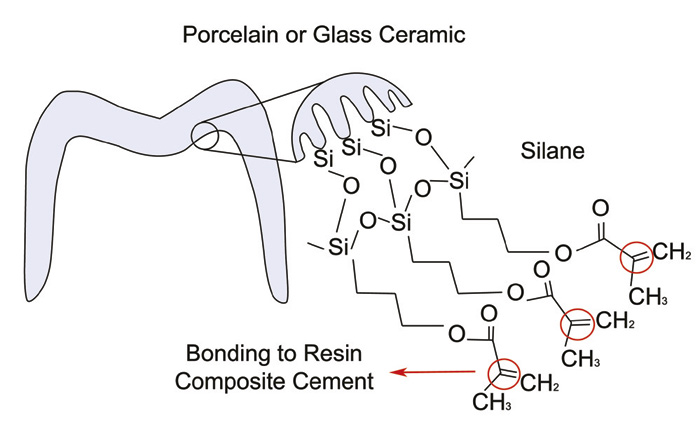
Figure 1. Chemical interaction of the silane with the etched surface of porcelain or glass ceramic restoration prior to application of the resin composite cement. (10) Note the formation of Si - O - Si bonds on the surface of the restoration. At the opposite end of the silane molecules, the methacrylate groups react with unreacted monomers in the resin composite cement by breaking of double bonds (circled in red).
Porcelain
Porcelains (feltspatic-, leucite- or fluorapatite-based) are capable of meeting the highest aesthetic standards but have limited mechanical properties. They are brittle, possess low fracture toughness and flexural strength when compared to glass ceramics and oxide-based ceramics, as a consequence of their very high glass content. Due to the material properties and the limited thickness in indirect restorations, the clinical success of porcelain veneers relies on reinforcement of the restorations by cementation. Cementation is vital because it creates strong and durable bonding, resulting from acid etching with HF plus silanisation and use of adhesive resin composite cements.
When etching with HF is performed at the dental laboratory, it occurs before testing the fit of the restoration in the mouth of the patient. In such cases, after testing the fit of the restoration on the patient, the surfaces to be cemented must be cleaned by the dentist with phosphoric acid, ethanol or a commercial product for cleaning ceramic, followed by rinsing, drying with (oil-free) compressed air and immediate silanisation. If HF etching is to be performed in the dental surgery, this is done after the restoration has been tested in the mouth of the patient, followed by rinsing, drying with compressed air, and silanisation. The time needed for silanisation (also often referred to as the drying time for silane) is, at minimum 1 min. (14).
Glass ceramics and reinforced glass ceramics
Glass ceramics have a wider application due to their improved mechanical properties with higher fracture strength and increased toughness compared to porcelain. Even if glass ceramics have different properties to porcelain, they still require adhesive cementation to reinforce the ceramic restoration. Among the group of glass ceramics, leucite-based or lithium disilicate-based are well known, while zirconia-reinforced glass ceramics are a more recent group. Zirconia-reinforced glass ceramics are, by definition, glass ceramics, with approximately 10 % zirconia blended in the matrix of lithium silicate (ZLS). The material has the same overall mechanical properties, with the same or slightly higher fracture strength but lower fracture toughness. Essentially, ZLS is an interesting alternative with the same indications as lithium disilicate-based glass ceramics. However, clinical studies and the knowledge of the material are, at present, limited.
Like porcelain, the surface pretreatment of glass ceramics, irrespective of their composition, is not dependent on the restoration production process and should include etching with HF, rinsing with water, drying with compressed air, and silanisation. A difference in the choice of cement is, however, that for thick or opaque glass ceramic restorations, a dual-cured adhesive resin composite cement should be chosen. Furthermore, if adequate micromechanical retention can be obtained through the tooth preparation and if the restoration fulfils the thickness requirements, a self-adhesive resin composite cement can be used.
A common question among clinicians is whether an extended time of HF etching on the restoration will create excessive superficial irregularities, so that this step would become the weak link if the restoration wall is very thin. The best advice is to follow the etching times recommended by the respective ceramic manufacturers (15,16).
Zirconia
The so-called pure oxide ceramics differ markedly from all other ceramic materials in chemical composition, with resulting high flexural strength, greater fracture toughness, and inertness. Such oxide ceramics, alumina (Al2O3) and zirconia (ZrO2) often defined as polycrystalline, high-strength ceramics, lack a glassy phase and are practically acid-resistant. Given this fact, oxide ceramics cannot be easily etched with HF. Conventional zirconia (also known as yttrium oxide, Y2O3, stabilised tetragonal zirconium dioxide polycrystals, Y-TZP) is less translucent than other ceramic materials. As development has focused on increasing zirconia's translucency, a newer generation of translucent zirconia is available (17). For new high-translucent zirconia, with lower fracture strength, proper bonding is more important and may be necessary for restorations fabricated at the minimum wall thickness threshold (18).
Conventional or translucent zirconia restorations can be bonded without pretreatment, but a physical surface pretreatment prior to cementation is strongly recommended. At present, the two most commonly used methods are based on grit-blasting, either using alumina powder or silica-coated alumina particles (tribochemical silica-coating). The first option is grit-blasting with alumina powder performed with an average particle size of 50 m, applied perpendicularly from a distance of about 10 mm, at a pressure of 1-2 bar (0.1-0.2 MPa), for 10-15 s. This pretreatment increases the surface roughness of the zirconia and enhances the mechanical interlocking (retention) for bonding. Alternatively, tribochemical silica-coating can be used: other than providing surface roughness, it creates an irregular silica layer on the ceramic surface when the special silica-coated alumina powder (average particle size for the Rocatec Soft ca.30 m and the Rocatec Plus ca. 110 m) is blasted at a perpendicular distance of 10 mm, under the pressure of 0.28 MPa. (10). Despite the benefits highlighted above of grit-blasting as a pretreatment of zirconia, this physical pretreatment, which depends mainly on the applied pressure (19) but to a lesser extent on the application angle (20), may introduce surface flaws that can, if at critical locations and under excessive stress, affect the long-term performance of the restoration.
For stronger bonding of adhesively cemented zirconia restorations, there are two options. If no pretreatment or grit-blasting using alumina powder is used, an adhesive resin composite cement system that contains 10-methacryloyloxydecyl dihydrogen phosphate (10-MDP) should be used. The grit-blasting with alumina powder is performed in the dental laboratory, followed by cleaning with water in an ultrasonic bath. Nevertheless, at the clinic - after testing the fit of the restoration on the patient - the restoration must be cleaned to remove contaminants (21) with especially developed products for zirconia (e.g. Ivoclean). Adhesive resin composite cements or ceramic primers containing 10-MDP are indicated because 10-MDP, the most promising functional monomer, forms a relatively stable chemical bonding with the demineralised tooth (through reaction between the hydrophobic 10-MDP parts with collagen) and with zirconia (through reaction between the phosphate ester groups of 10-MDP with the hydroxyl groups on the passive zirconia surface) (Fig. 2) (22,23). The 10-MDP to collagen complexation may contribute to the generally well-performing 10-MDP-based self-adhesive cements. When choosing an adhesive resin composite cement to bond to zirconia, dual- or chemical curing is necessary. This because it is very difficult for the blue light to access the cement layer, due to the material's reduced translucency and minimum required thickness.
Alternatively, if tribochemical silica-coating is employed, it should be followed by rinsing, air drying and the application of silane, which enables chemical adhesion to any resin composite adhesive cement (24). However, a significant loss in bond strength over the long-term, following pretreatment with tribochemical silica-coating and silane, as reported when using traditional resin composite cements, further supports the use of phosphate monomer-containing adhesive resin composite cements for luting of zirconia (24).
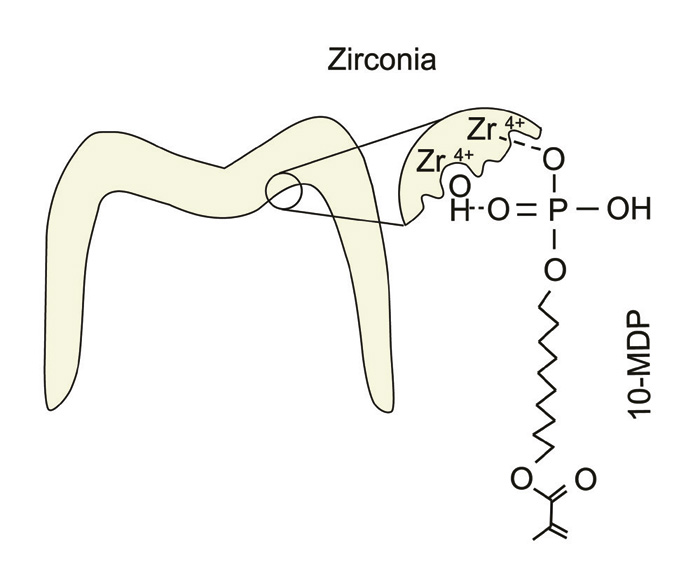
Figure 2. Chemical interaction of the 10-MDP monomer with the roughed zirconia surface obtained by grit-blasting. Ionic and hydrogen bonding may occur between 10-MDP and zirconia - here both possibilities are illustrated, but they may also occur separately. (23)
Clinically relevant aspects for luting ceramic restorations
When choosing the type of resin composite cement to be used, the type of ceramic material is the starting point. As already mentioned above, a homogeneous, well-bonded, and defect-free adhesive cement layer minimises the risk of fracture of porcelain or glass ceramic restorations (1,2). In fact, a clinical follow-up of lithium disilicate crowns during 9 years of service in the mouth shows a reduced success rate when these crowns were luted with a resin-modified glass ionomer cement, compared to luting with a resin composite cement (25).
Type of pretreatment |
Ceramic material |
||
|---|---|---|---|
Porcelain |
Glass ceramics |
Oxide-based ceramics,Zirconia* |
|
Physical pretreatment |
None |
None |
Grit-blasting with alumina powder (1st option) or silica-coated alumina particles (2nd option) |
Chemical pretreatment |
Hydrofluoric acid etching + silanisation |
Hydrofluoric acid etching + silanisation |
Tribochemical silica coating + silanisation (2nd option) |
* If zirconia is cemented as produced, then an adhesive cement system containing 10-MDP is strongly recommended.
Other than strengthening of the restoration, it is also important to consider the aesthetics during the planning phase. In the anterior region, for highly aesthetically demanding cases, particularly if the more translucent porcelain or glass ceramics are to be used, current adhesive resin composite cement systems offer a wide range of shades. A number of manufacturers provide the so-called try-in pastes, (for use while testing the restoration fit), to aid the clinician in choosing the best matching shade of the cement, before the restoration is finally cemented. A translucent shade, however, is sufficient to bond highly skilled restorations, which already take into account the colour of the prepared tooth and the neighbouring teeth. For such translucent restorations in the anterior region, it is essential to choose an adhesive resin composite cement system which shows good colour stability. Dual-cured resin composite cements that contain a tertiary amine suffer significantly more marginal discoloration with ageing than the light-cured resin composite cements (26,27). This said, an amine-free resin composite cement should be used for luting anterior, translucent ceramic restorations (Table 2). Resin composite cements that are exclusively light-cured, amine free, and deemed more colour-stable (26), are therefore indicated to bond such restorations as long as the ceramic thickness does not exceed 2 mm (28). Otherwise, an amine-free dual-cured resin composite cement is advised. This is because the light irradiance and total energy reaching the cement are significantly reduced when light-curing takes place through ceramics (29,30). Regardless of choosing light- or dual-cured adhesive resin composite cements for luting translucent ceramic restorations, adequate light-activation is needed to maximise the cements' degree of conversion and mechanical properties (31).
Ceramic material |
|||
|---|---|---|---|
Porcelain |
Glass ceramics |
Zirconia |
|
Type of adhesive cement system |
Light or dual-cured (preferably amine-free) resin composite cement |
Light or dual-cured (preferably amine-free) resin composite cement |
Dual- (or chemically) cured resin composite cement containing 10-MDP.Alternatively resin-modified glass ionomer cement. |
10-MDP = 10-methacryloyloxydecyl dihydrogen phosphate
Adhesive cementation can be recommended even when stronger ceramics, i.e. zirconia, are used. The latter can be particularly beneficial in cases where the height of the preparation is too short or if the preparation has convergence angles larger than the optimal recommendation, in which case mechanical retention becomes compromised (32). For bonding the more opaque zirconia, a dual- (or chemically) cured resin composite cement needs be used (Table 2). The choice of a dual-cured self-adhesive resin composite cement is advantageous: it simplifies the procedure as no pretreatment of the teeth (other than comprehensively cleaning the residues of the temporary cement) is needed and if 10-MDP is present, it is beneficial for the bond strength (33-35). Considering oxide ceramics, similar survival rates, after an observation period of up to 8 years, for single crowns have been reported, regardless of the choice of cement, with a slightly higher tendency for loss of retention by luting with zinc phosphate when compared to resin-modified glass ionomer cement (36) or self-adhesive resin composite cement (37). Nevertheless, it should be emphasised that clinical long-term studies indicate that oxide ceramic crowns and FDPs also have high long-term survival rates when luted with conventional cements (18). Even so, most studies recommend bonding zirconia with self-adhesive resin composite cements, which have today virtually substituted the use of zinc phosphate cements.
The available clinical evidence proposes that successful bonding of zirconia restorations can be achieved, but the durability of the bond is variable (38). Clinical studies on non-retentive resin-bonded fixed prosthesis - or those with limited mechanical retention - are thus considered the perfect in vivo test case to truly assess bonding to zirconia. In a review conducted by Kern (38), studies reported less debonding in such non-retentive zirconia restorations - varying between 4.8 % to 7.1 % and caused only by traumatic incidents - if grit-blasting (using 50 m alumina powder at 2.5 bar) followed by luting with a MDP-containing resin cement were chosen, during an observation period of 20-64 months. These results are supported by a recently published clinical study on non-retentive zirconia, cantilever resin-bonded fixed dental prostheses that were grit-blasted (using 50 m alumina powder at 1.0-2.5 bar) prior to cementation. In the latter study, 4.2 % debonding was registered in restorations luted with a MDP-containing resin cement (Panavia 21 TC), while 14.2 % debonding occurred in restorations luted with a methacrylate-based resin cement (Multilink Automix), during 10 years of observation (39). The above mentioned results (38,39), corroborated by laboratory testing (24,40), support the use of grit-blasting combined to a MDP-containing resin cement for durable bonding to zirconia.
On the other hand, the review identified that if the surface of the zirconia was used as produced - only cleaned with ethanol - and luted using both a MDP-containing primer and resin cement, 13.3 % debonding occurred during normal function in a period of 53 months, even for a more retentive restoration design. Additionally, significantly higher debonding (46.2 %) was identified for inlay-retained zirconia restorations after tribochemical silica coating, silanization and luting with a MDP-containing resin cement during a 12-month follow-up - thus indicating a weak link between the silica layer and zirconia (38). These results suggest that tribochemical silica coating and silane application may not lead to durable bond to zirconia.
Additional clinical parameters are relevant when choosing the cement for luting ceramic crowns. Ease of handling and appropriate working times are important characteristics. A successful cementation is also dependent on the proper handling of materials (we need to read the instructions for use carefully) and surface pretreatment of the restoration and dental tissues (41). It is therefore very important to adhere to recommendations from the manufacturers as regards their bonding agents, ceramic primers, and adhesive resin composite cements. It is also vital to strictly adhere to the same bonding and cementation system, not interchanging products from different manufacturers with different chemical compositions that may not be at all compatible with each other (18).
Final comments
Regardless of the choice of ceramic material, the adhesive resin composite cement system, and surface pretreatment methods, it is vital for the dentist and dental technician to become confident with the use of the chosen treatment modality, the materials and working methods.
References
Fleming GJP, Addison O. Adhesive cementation and the strengthening of all-ceramic dental restorations. J Adhes Sci Technol 2009; 23: 945-59.
Fleming GJP, Cao X, Romanyk DL et al. Favorable residual stress induction by resin-cementation on dental porcelain. Dent Mater 2017; 33: 1258-65.
Mallineni SK, Nuvvula, S, Matinlinna JP et al. Biocompatibility of various dental materials of contemporary dentistry: a narrative insight. J Investig Clin Dent 2013; 4: 9-19.
Ekambaram M, Yiu CY, Matinlinna JP. Bonding of adhesive resin to intraradicular dentin - a review of the literature. Int J Adhes Adhes 2015; 60: 92-103.
Ekambaram M, Yiu CY, Matinlinna JP. Bonding of resin adhesives to caries-affected dentin - a systematic review. Int J Adhes Adhes 2015; 61: 23-34.
Matinlinna JP, Lung CYK, Tsoi JKH. Silane adhesion mechanism in dental applications and surface treatments: a review. Dent Mater 2018; 34: 13-28.
Papia E, Larsson C, du Toit M et al. Bonding between oxide based ceramics and adhesive cement systems: A systematic review. J Biomed Mater Res B Appl Biomater 2014; 102: 395-413.
Ho GW, Matinlinna JP. Insights on ceramics as a dental material. Part I: Ceramic material types in dentistry. Silicon 2011; 3: 109-15.
Ho GW, Matinlinna JP. Insights on ceramics as a dental material. Part II: Chemical surface treatments. Silicon 2011; 3: 117-23.
Lung CYK, Matinlinna JP. Chapter 11: Surface pretreatment methods and silanization. In: Matinlinna JP (ed.). Handbook of Oral Biomaterials. Singapore: Pan Stanford Publishing, 2014; 359-98.
Özcan M, Matinlinna J. Surface conditioning protocol for the adhesion of resin-based cements to base and noble alloys: how to condition and why? J Adhes Dent 2015; 17: 372-3.
Lung CY, Matinlinna JP. Aspects of silane coupling agents and surface conditioning in dentistry: an overview. Dent Mater 2012; 28: 467-77.
Matinlinna JP, Lassila LVJ, Vallittu PK. Evaluation of five dental silanes on bonding a luting cement onto silica-coated titanium. J Dent 2006; 34: 721-6.
Özcan M, Matinlinna JP, Vallittu PK et al. Effect of drying time of 3-methacryloxypropyltrimethoxysilane on the shear bond strength of composite resin to silica-coated base/noble alloys. Dent Mater 2004; 20: 586-90.
Hooshmand T, Matinlinna JP, Keshvad A et al. Bond strength of a dental leucite-based glass ceramic to a resin cement using different silane coupling agents. J Mech Behav Biomed Mater 2013; 17: 327-32.
Lanza MDS, Lanza FJSR, Manso AP et al. Innovative surface treatments for improved ceramic bonding: lithium disilicate glass ceramic. Int J Adhes Adhes 2018; 82: 60-6.
Li RW, Chow TW, Matinlinna JP. Ceramic dental biomaterials and CAD/CAM technology: state of the art. J Prosthodont Res 2014; 58: 208-16.
Blatz MB, Vonderheide M, Conejo J. The effect of resin bonding on long-term success of high-strength ceramics. J Dent Res 2018; 97: 132-9.
Heikkinen TT, Lassila LVJ, Matinlinna JP et al. Effect of operating air pressure on tribochemical silica-coating. Acta Odontol Scand 2007; 65: 241-8.
Ho BJ, Tsoi JKH, Liu D et al. Effects of sandblasting distance and angles on resin cement bonding to zirconia and titanium. Int J Adhes Adhes 2015; 62: 25-31.
Yang B, Scharnberg M, Wolfart S et al. Influence of contamination on bonding to zirconia ceramic. J Biomed Mater Res B Appl Biomater 2007; 81: 283-90.
Inokoshi M, De Munck J, Minakuchi S et al. Meta-analysis of bonding effectiveness to zirconia ceramics. J Dent Res 2014; 93: 329-34.
Nagaoka N, Yoshihara K, Feitosa VP et al. Chemical interaction mechanism of 10-MDP with zirconia. Sci Rep 2017; 7: 45563.
Thompson JY, Stoner BR, Piascik JR et al. Adhesion/cementation to zirconia and other non-silicate ceramics: where are we now? Dent Mater 2011; 27: 71-82.
Gehrt M, Wolfart S, Rafai N et al. Clinical results of lithium-disilicate crowns after up to 9 years of service. Clin Oral Investig 2013; 17: 275-84.
Almeida JR, Schmitt GU, Kaizer MR et al. Resin-based luting agents and color stability of bonded ceramic veneers. J Prosthet Dent 2015; 114: 272-7.
Marchionatti AME, Wandscher VF, May MM et al. Color stability of ceramic laminate veneers cemented with light-polymerizing and dual-polymerizing luting agent: a split-mouth randomized clinical trial. J Prosthet Dent 2017; 118: 604-10.
Blatz MB, Sadan A, Kern M. Resin-ceramic bonding: a review of the literature. J Prosthet Dent 2003; 89: 268-74.
Pereira CN, De Magalhães CS, Daleprane B et al. LED and halogen light transmission through a CAD/CAM lithium disilicate glass-ceramic. Braz Dent J 2015; 26: 648-53.
Faria-E-Silva AL, Pfeifer CS. Effectiveness of high-power LEDs to polymerize resin cements through ceramics: an in vitro study. J Prosthet Dent 2017; 118: 631-6.
Aguiar TR, de Oliveira M, Arrais CA et al. The effect of photopolymerization on the degree of conversion, polymerization kinetic, biaxial flexure strength, and modulus of self-adhesive resin cements. J Prosthet Dent 2015; 113: 128-34.
Heintze SD. Crown pull-off test (crown retention test) to evaluate the bonding effectiveness of luting agents. Dent Mater 2010; 26: 193-206.
Peutzfeldt A, Sahafi A, Flury S. Bonding of restorative materials to dentin with various luting agents. Oper Dent 2011; 36: 266-73.
Benetti AR, Peutzfeldt A. Bindingssystemer og deres anvendelse. Tandlægebladet 2016; 120: 1000-6.
Ubaldini ALM, Benetti AR, Sato F et al. Challenges in luting fibre posts: adhesion to the post and to the dentine. Dent Mater 2018; 34: 1054-62.
Jokstad A. A split-mouth randomized clinical trial of single crowns retained with resin-modified glass ionomer and zinc phosphate luting cements. Int J Prosthodont 2004; 17: 411-6.
Örtorp A, Kihl ML, Carlsson GE. A 5-year retrospective study of survival of zirconia single crowns fitted in a private clinical setting. J Dent 2012; 40: 527-30.
Kern M. Bonding to oxide ceramics - laboratory testing versus clinical outcome. Dent Mater 2015; 31: 8-14.
Kern M, Passia N, Sasse M et al. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J Dent 2017; 65: 51-5.
Passia N, Mitsias M, Lehmann F et al. Bond strength of a new generation of universal bonding systems to zirconia ceramic. J Mech Behav Biomed Mater 2016; 62: 268-74.
Manso AP, Silva NR, Bonfante EA et al. Cements and adhesives for all-ceramic restorations. Dent Clin North Am 2011; 55: 311-32.
Corresponding author: Ana R. Benetti, Nørre Allé 20, Copenhagen N, DK-2200, Denmark. E-mail: arbe@sund.ku.dk
Conflicts of interest: The authors declare no conflicts of interest.
This paper has been peer reviewed.
Benetti AR, Papia E, Matinlinna JP. Bonding ceramic restorations. Nor Tannlegeforen Tid. 2019; 129: 30-36
associate professor, ph.d., Division of Dental Materials, Department of Odontology, Faculty of Health and Medical Sciences, University of Copenhagen
assistant professor, ph.d., Department of Materials Science and Technology, Faculty of Odontology, Malmö University
professor, ph.d., Department of Dental Materials Science, Faculty of Dentistry, University of Hong Kong