Clinical outcomes of ceramic restorations
This paper addresses the available recent clinical evidence for different treatment possibilities with ceramic materials. Furthermore, an analysis of the failures occurring and the reason for these is discussed. The paper focuses on single and multi-unit restorations (fixed dental prostheses, FDPs) supported on teeth or implants.
The survival of ceramic restorations is favourable and comparable with metal ceramic ones. Biological complications are rare. The cause-effect relationship is multifactorial and mostly influenced by host-related factors rather than by the type of restorative material. Fractures are the main technical complications. Margin fractures is the most common complication for crowns, and connector fractures for FDPs.
Headlines | |
|---|---|
· |
The survival of ceramic restorations is favourable and comparable with metal ceramic ones when used on appropriate indications. |
· |
Biological complications are rare. The cause-effect relationship is multifactorial and mostly influenced by host-related factors rather than by the type of restorative material. |
· |
Fractures are the main technical complications. |
Introduction
There is a plethora of ceramic materials available for clinicians to choose from, but limited scientific evidence to show which material is best in each specific case. There has been a steady increase in the number of clinical trials with ceramic materials, but there is still few randomized clinical trials, which are regarded as the highest level of evidence. Large differences in study population, methods used, success and survival criteria and follow-up time among the different prospective and retrospective clinical trials make comparison among the materials and treatment options difficult. This paper addresses the available recent clinical evidence for different treatment possibilities with ceramic materials. Furthermore, an analysis of the failures occurring and the reason for these are discussed.
When assessing clinical success, there are several criteria that need to be addressed. Most clinical trials report survival rates, but with no further disclosure of what is regarded as «survival» (1). Survival can thus mean everything from «no problems at all» to the restoration is «still in place» (Figure 1). According to Tan et al. (2), a survived restoration is still in use at the follow-up time, with or without reversible complications.
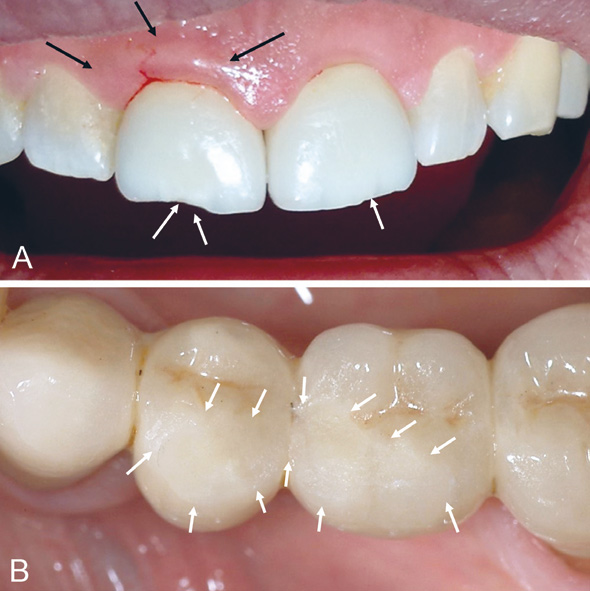
Figure 1, A-B. A: Examples of surviving restorations that are not entirely successful due to minor or reversible complications. Gingivitis as a result of cement residue, black arrows. The lesion healed after polishing. Minor incisal chipping that could be polished, white arrows. Photo: Ritva Näpänkangas. B: Multiple superficial veneer chipping defects on a FDP still in function, white arrows indicate the extent of the defect. Photo: Christel Larsson.
Success, however, is used as term for «a restoration with no complications during the observation period,» (2). Patient satisfaction is surprisingly seldom included in the evaluation. There are reasons to believe that every-day practices have lower success rates than what is generally reported in clinical trials where specialists with ample time perform the prosthetic treatment.
Survival of tooth-supported single unit crowns
Several systematic reviews have evaluated the success and survival of ceramic single unit restorations (3-5), but very few studies have more than 5 year's follow-up. When considering the success and survival of different materials and restoration types one must take into consideration that they are often made based on very different indications and conditions. Some reviews include meta-analyses where all the individual data from each of the included studies were similar enough to be put into one large pool for increased power of the statistical analyses. The meta-analysis has showed the survival rates of single unit ceramic crowns to be similar to metal ceramic ones with a 5 year survival rate of 94 % (5). Metal-ceramics is still considered as a «gold standard» with regard to clinical evidence. The posterior ceramic crowns seem more likely to fail than anterior crowns (5).
Veneers and adhesively cemented porcelain crowns
The use of shell-like adhesively cemented porcelain crowns and buccal veneers is well documented in multiple studies (6,7). The survival rates are high; around 90 % over 5-10 years and complications are few. Fractures are the most common complication (4 %), followed by debonding (2 %) and secondary caries (1 %). More complications occur when the preparation border extends beyond enamel or when cementation is performed without sufficient control of humidity. The restorations evaluated in these studies are mostly in the anterior region and on teeth with no or moderate previous damages which would significantly improve ease of maintenance and the potential for success and survival. Porcelains are used in veneered bi-layer ceramics and in metal-ceramics, as well as in aesthetic veneers and shell-like crowns, where glass-ceramics and zirconia cannot satisfy the need for optimal aesthetics.
Inlays-onlays
The survival and success of inlays and onlays have been studied in multiple trials (8). The overall 10-years survival rates are around 90 %. There are, however, large discrepancies in inclusion and exclusion criteria in the different studies, ranging from small MOD-inlays to large onlays which are closer to 3/4 crowns and so called «table-top» onlays for severely worn dentitions. Early trials of chair-side produced inlays show relatively high complication rates with marginal chipping, discoloration and secondary caries as common complications (9). The intra-oral scanning and CAD/CAM production has improved immensely since the introduction in the 1990's, however, and the success rates are naturally improving as a consequence. Fractures are the most common complication (4 %), followed by endodontic complications (3 %) and secondary caries (1 %) and debonding (1 %) (8).
Glass-ceramic crowns
Lithium- disilicate (LiO2) reinforced glass-ceramic crowns are among the best-documented treatment choices for restoring teeth in terms of number of published clinical trials (10). Based on a meta-analysis of a large number of restorations, the estimated 5-year survival rate of glass ceramic (leucite or lithium-disilicate reinforced) restorations was 96.6 %, whereas glass infiltrated alumina crowns had an estimated 5-year survival rate of 94.6 %. The long-term success is, however, less certain as few studies have more than 5 years follow-up. Again, one must consider that the information of the previous condition of the restored teeth in the different studies is limited, and it is thus difficult to compare the survival rates for each separate case.
Zirconia and Alumina (polycrystalline ceramics)
Alumina crowns were for many years the most used ceramic restorations in the Nordic countries. Studies of alumina crowns have shown a 5-year survival rate of approximately 93 % (3-5). Based on personal reports and feedback from dental technicians, the complication rates were significantly higher than reported in scientific publications. Both crown loosening and fractures have been experienced frequently. Alumina has been more or less totally replaced by zirconia over the last 10 years as the material of choice for ceramic restorations for teeth with moderate to substantial loss of substance and need for strong material. Relatively few clinical prospective studies on single unit zirconia crowns have been performed, but some recent reports indicate a 96 % 5-year survival rate, but with a significant drop in survival in the following two years to 75 %-93 % (11-14). Two retrospective studies based on dental laboratory data from up to 5 years of production show fracture rates of 3.35 % for bi-layered crowns and 2.0 per cent for monolithic restorations (15-16).
Few studies have exceeded mean five-year follow-up time in ceramic restorations. It should be kept in mind that the improvement of ceramic materials has developed quickly in recent years and the results of the long follow-up studies may include old materials. So far, there is no clinical documentation above one year of the clinical performance of translucent or high-translucent zirconia (cubic/anterior) materials that are recently introduced.
Survival of tooth-supported fixed dental prostheses (FDPs)
Two recent systematic reviews have addressed the survival rates of tooth-supported FDPs (17-18). Both found that the difference between ceramic and metal-ceramic restorations was not statistically significant after 5 years follow-up. The estimated survival rate of reinforced glass ceramics was 89.1 %, whereas glass-infiltrated alumina had 86.2 % and zirconia approximately 91 %. The survival rate of metal-ceramic FDPs was 94.4 % after five years. Regarding zirconia, long-term (7-10 years) follow-up studies have been published for multi-unit FDPs and the survival rate ranges from 75-100 % (12, 19-21). Veneer chipping was the predominant complication in the earlier studies.
Resin bonded ceramic fixed dental prostheses (RBFDPs)
Ceramic resin retained FDPs have previously been rather unsuccessful. Resent development in bonding to zirconia shows, however, promising results. One study of 108 zirconia restorations restoring missing incisors showed a survival rate of 98 % after ten years (22). Of these 108 restorations, six had debonded, but all could be rebonded successfully. It is important to note that only one wing was used for retainer in both these trials. Furthermore, a special attention was made to follow a strict protocol in order to achieve sufficient bonding. Trials with ceramic RBFPDs with two wings have significantly lower success rates, since both fractures and loss of retention is experienced more frequently for two-winged restorations (23). There are however very few publications and further results should be awaited.
Survival of implant-supported single crowns
A survival of 97.1 %-100 % has been reported for implant-supported ceramic crowns after three to five years (14,24-25). Both monolithic lithium disilicate implant-supported single crowns, and monolithic zirconia crowns have been studied. Even though the survival was high in all studies, the success rates was significantly lower (87.5 %-91.7 %), indicating that there was or had been complications with the restorations within the follow-up.
Survival of implant-supported FDPs
Five-year survival rate of implant-supported zirconia-based FDPs has been found to be 100 % in two studies with zirconia-based restorations, bi-layered (18) and monolithic (24). The number of patients were, however, low and the results must be regarded with caution.
Biological complications
Tooth-supported restorations
As mentioned above, the success/survival rate of ceramic restorations is favourable. Biological complications are rare and seldom exceed a prevalence of 2 % in 5 years (3,4,17,27). The early complications with ceramic restorations are more often biological than technical, however, and can be related to excess cement in marginal areas (28). Biological complications seem to be unrelated to type of restoration and material (3-4,27). Glass-infiltrated alumina crowns have in some studies showed higher incidence of caries, but ceramic crowns, in general, perform better than metal-ceramic crowns, from a biological perspective (3). In another study, there was a statistically significant higher prevalence of periodontal disease among multi-unit FDPs made of glass-infiltrated alumina and glass-ceramics, compared to metal-ceramic FDPs (17). In addition, there was a significantly higher prevalence of caries among FDPs made of zirconia compared to metal-ceramic FDPs. The authors did not discuss the differences in prevalence of periodontal disease but explain the differences in caries prevalence by suggesting a relationship between caries and the fit of a restoration, which was suboptimal in the beginning due to limitations in precision manufacturing in the early years of zirconia manufacturing.
Some of the biological complications associated with ceramic multi-unit-restorations may be associated with the increased connector sizes necessary for strength of the material. This leaves less space for interproximal cleaning procedures and thus increased risk for plaque-associated diseases. Furthermore, the bi-layer design, still favoured in anterior regions, may result in slightly over-contoured restorations, which complicates plaque removal.
Implant-supported restorations
Information from clinical trials on implant-supported ceramic restorations is scarce. The type of prosthetic material does not seem to influence implant or prostheses survival and complication rate (29). Other reviews mainly focus on zirconia-based restorations (14, 18). As for tooth-supported restorations, biological complications are rare. For single crowns, some bleeding on probing has been noted (14), but no biological complications were noted among FDPs (18). Ceramics are also popular as materials for implant abutments. Whether ceramic abutments may influence prevalence of biological complications is unknown. A review comparing metal and ceramic abutments found lower prevalence of biological complications around ceramic abutments but the difference was not statistically significant (30).
The findings that biological complications are rare is encouraging. Ceramic materials have been found to accumulate less plaque and plaque with reduced vitality, compared to other restorative materials, but the clinical significance is uncertain (31-32). Biological complications include a range of different diseases: e.g. caries, periodontal and endodontic diseases, where the cause-effect relationship is multifactorial and mostly influenced by host-related factors rather than factors such as type of restorative material.
None of the reviews mentioned adverse reactions to dental materials. Ceramic materials show excellent biocompatibility in comparison to most metals (Anusavice book). However, even though the prevalence of metal allergies is relatively high in the general population, clinical manifestations are rare and potential risks should not be overemphasized (34, 35). For the small number of patients with a known sensitivity to metals, ceramic materials, or titanium and titanium alloys, may be advantageous.
Technical complications
As discussed above, most published clinical trials have relatively low rates of technical failures. Fractures remain the most common technical complication, and are responsible for between 0.5 to nearly 6 % annual complication rates in different studies, depending on fracture mode and the type of the restoration (single or FDPs, supported on teeth or implants) (3, 17). There are two main types of fracture modes, fractures in the veneering material (chipping) and core fracture (total fractures or catastrophic fractures). These can be further divided into four fracture modes based on localization and severity (Figure 2). It is, however, uncertain whether the success rates are equally good in normal everyday practices. Based on communication with practicing dentist and dental technicians, fractures remain a clinical problem. A large British registry of revision rates and survival of dental restorations from regular dental practices showed that ceramic crowns have a shorter time in clinical function than metal-ceramic ones (36). The exact reason is not evident based on the registry, but fractures are considered the major contributing factor. Crown loosening is the other major technical complication with annual failure rates between 0.11 % and 1 % in different studies (3, 17). The lack of periodontal receptors surrounding the implants can probably explain the high technical complication rates (most commonly chip-off ceramic fractures) in implant-based restorations due poorer chewing precision and thus to higher mastication loads compared to natural teeth. Furthermore, implant-based restorations often have long coronal height compared to tooth-based restorations creating unfavorable force vectors.
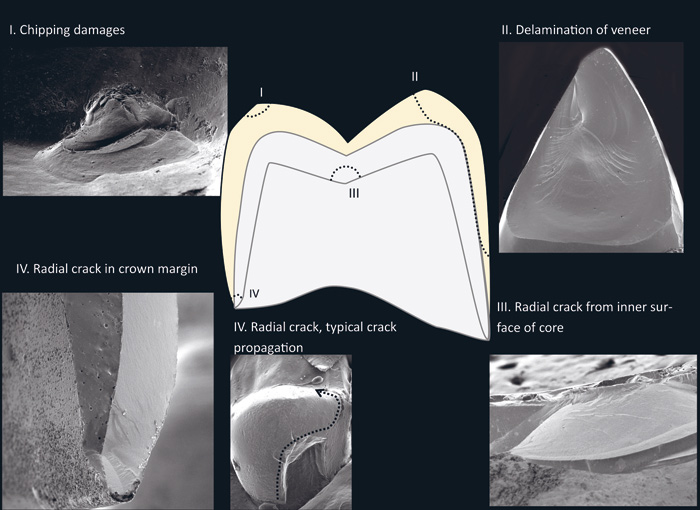
Figure 2. Different fracture types observed in clinical failures. I) chipping, II) delamination of veneering ceramic, III) cracks originating in the inner surface of the crown, IV) cracks originating from the crown margin. Photo. Marit Øilo.
Most papers involving systematic fractographic analyses of the fractures of retrieved dental crowns that have failed during clinical practices are case reports or case series. Retrieval of crowns failed by chipping is difficult without destroying the remaining restoration. Furthermore, chipped veneer is often adjusted in situ instead of being replaced as long as function or aesthetics is not severely reduced. Core failures are easier to collect and a relatively large number of cases has been identified by several authors (37-45)
The prevalent assumption has been that ceramic crowns fail due to contact damage at the point of occlusion. However, analyses of retrieved crowns reveal that most clinical crowns produced of modern ceramics with core failures originate from cracks starting in the cervical margin, and usually in the approximal area or in the palatinal region (Figure 3). Some crowns fracture from inner radial cracks, sometimes referred to as cone cracks, in the area opposing the occlusal load (Figure 4). Chipping failures, on the other hand (Figure 5), seem to originate from poor veneer support, traumatic occlusion, improper occlusal adjustments, defects or pores in the veneering material or accidental biting on hard objects (46-48). Chipping failures are more commonly observed on implant-based than in tooth-supported restorations. Additionally, fractures of zirconia abutments have been observed, but the occurrence rates are uncertain (Figure 6). The number of restorations analyzed by standardized fractographic analyses is, however, not yet large enough to draw any definitive conclusions concerning the cause-effect relationship of clinical fractures overall. The restorations analyzed vary greatly in size, shape and materials used. The fracture may be caused by many factors, such as; wear, grinding, material flaws, residual stress, thin margins, machining cracks or a combination of two or more factors (49). Multi-unit restorations, on the other hand, mostly break in the connector area. The few publications addressing this, reveal that the connector areas in fractures restorations are very often poorly designed, with sharp angles or asymmetric shape, and smaller than recommended. Furthermore, grinding marks causing cracks are often evident (Figure 7). Based on the existing publications, it can be concluded that margin initiated fracture is a fairly common failure mode for core fracture of crowns. FDPs fracture due to poorly dimensioned connectors. Traumatic occlusion or poor occlusal adjustment are common causes of chipping.
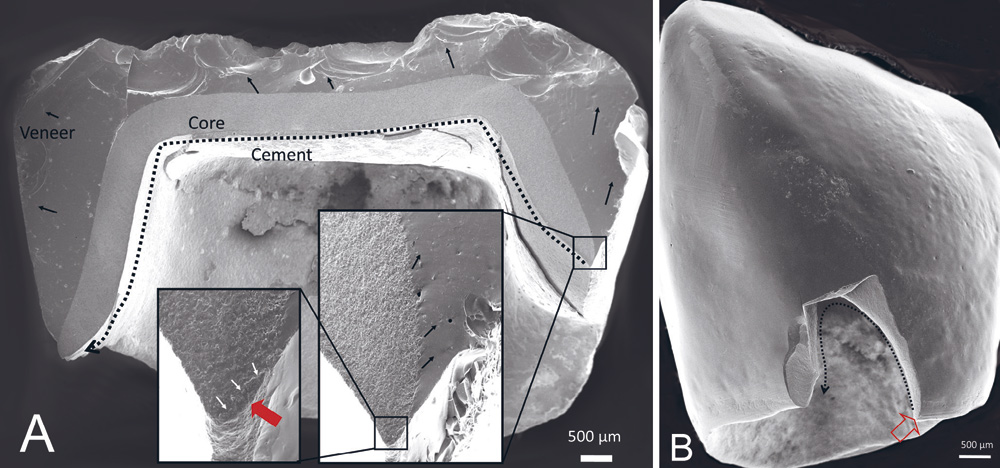
Figure 3, A-B. A: A typical clinical core-veneer crown failure mode. The fracture starts in the cervical margin and propagates through the crown across the occlusal surface, splitting the crown in two. Red arrow indicate fracture origin. B: Typical failure mode for monolithic crowns. A small semicircular part has broken off from the margin. Red arrow indicate fracture origin. Photos. Marit Øilo.
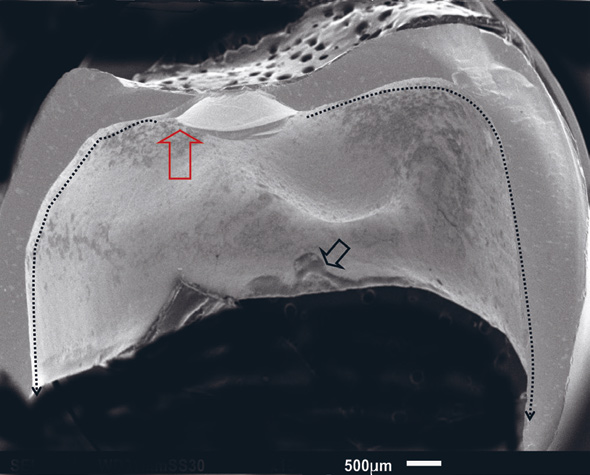
Figure 4. A monolithic zirconia crown fractured in two in clinical use. The fracture origin (red arrow) is in the inner surface of the occlusal wall. Photo: Marit Øilo.
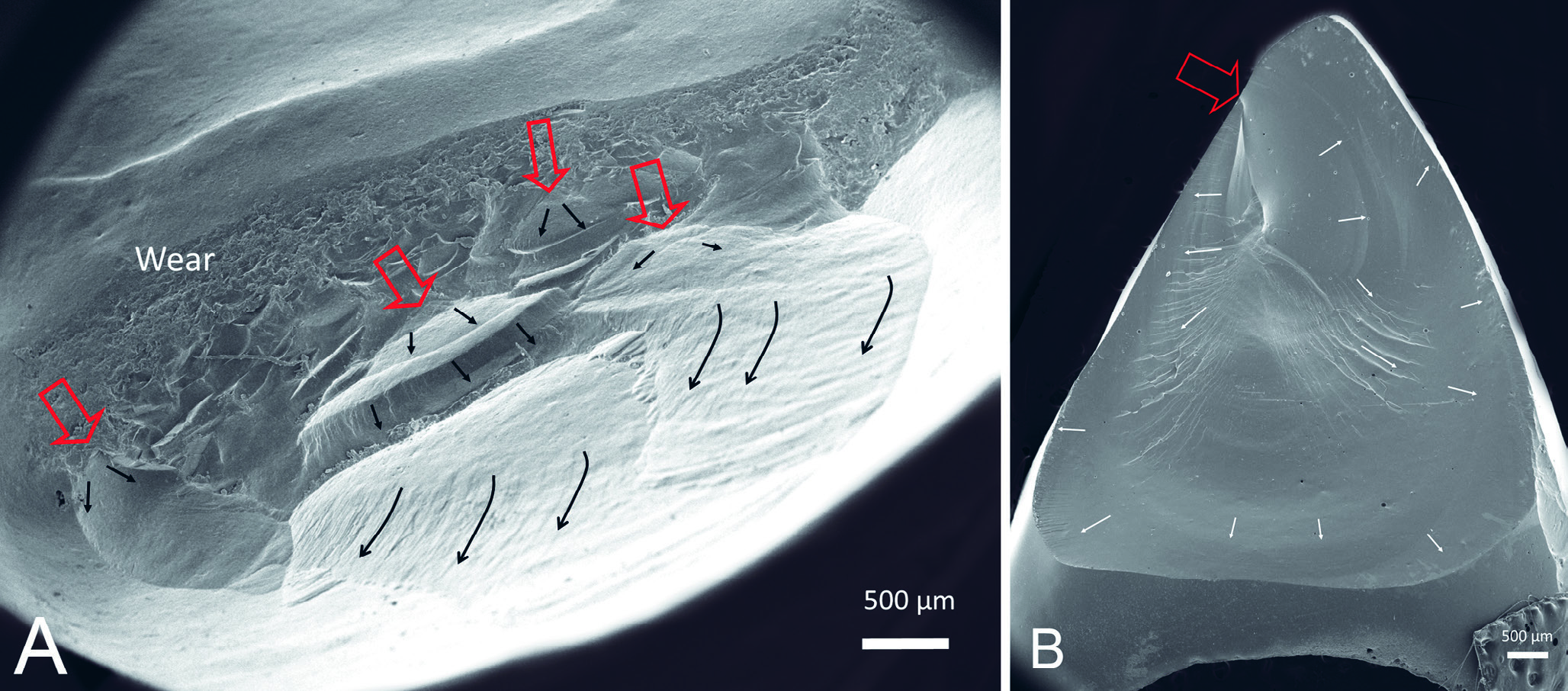
Figure 5, A-B. A: Typical chipping and B: delamination fractures. Both seem to be initated (red arrowns) by wear and poor veneer support. Photo. Marit Øilo.
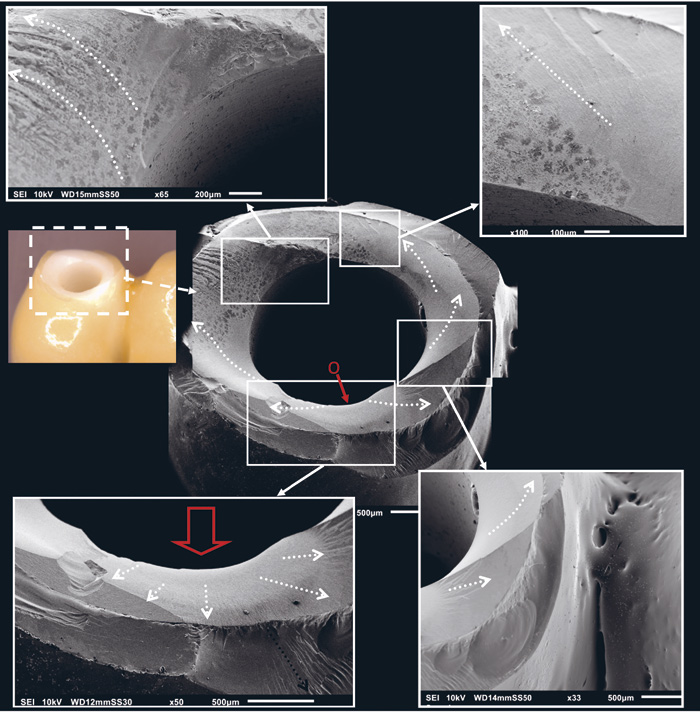
Figure 6. Fractured implant based crown, where the fracture started on the inside of the abutment (red arrow) due to high bending forces. Photo. Marit Øilo.
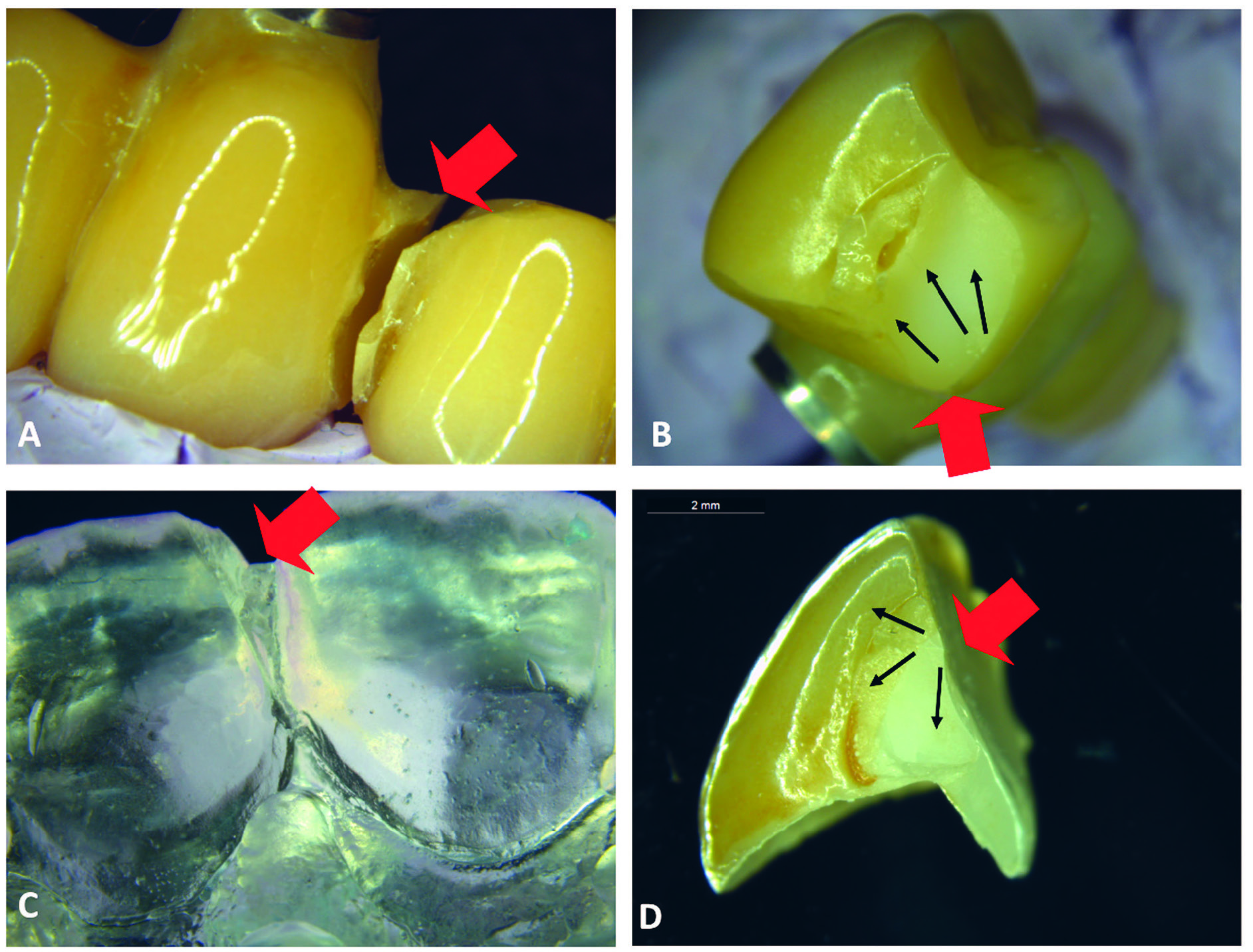
Figure 7, A-D. Multi-unit restorations most often fracture in the connector areas. Fractographic analyses often reveal poorly dimensioned connectors with unfavorable design causing stress concentrations in narrow parts. Furthermore several cases have revealed grinding damages in the connector area below the veneering ceramic. A: An implant based 4-unit restoration fractures in the connector area (red arrow). B: The connector in severely under dimensioned. C: A three-unit tooth retained restoration fractured between abutment and connector (red arrow, epoxy model based on impression taken in situ, before removal of restoration). D: the connector area is poorly designed, and the sharp edge towards the incisal edge caused stress concentration in this region (red arrow).
The cause for crown loosening is, unfortunately, seldom included in scientific publications. There can be many reasons for crown loosening: poor retention form of the abutment, too thick cement space, improper use of cement, contamination of surfaces or poor adhesion between cement and the surfaces in restoration or tooth. All of these factors can be at play for ceramic crowns. The need for rounded edges and finish lines reduces the area available for mechanical retention. Furthermore, there is still debate regarding the efficiency of adhesive bonding to alumina and zirconia, although Kern et al. have shown very promising clinical results with their method for bonding to zirconia (50).
Conclusion
Despite the fact that the ceramic materials available today are stronger and more versatile than ever, failures do occur in clinical use. Although biological complications are rare compared to metal-ceramic restorations, technical complications occur at similar or on higher level than for metal-ceramic restorations. Choosing the right material for each case and proper handling of the materials is crucial and can reduce the number of complications.
References
Anusavice KJ. Standardizing failure, success, and survival decisions in clinical studies of ceramic and metal-ceramic fixed dental prostheses. Dent Mater. 2012; 28: 102-11.
Tan K, Pjetursson BE, Lang NP, Chan ES. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res. 2004; 15: 654-66.
Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent Mater. 2015; 31: 603-23.
Aldegheishem A, Ioannidis G, Att W, Petridis H. Success and Survival of Various Types of All-Ceramic Single Crowns: A Critical Review and Analysis of Studies with a Mean Follow-Up of 5 Years or Longer. Int J Prosthodont. 2017; 30: 168-81.
Kassardjian V, Varma S, Andiappan M, Creugers NH, Bartlett D. A systematic review and meta analysis of the longevity of anterior and posterior all-ceramic crowns. J Dent. 2016; 55: 1-6.
Layton DM, Clarke M. A systematic review and meta-analysis of the survival of non-feldspathic porcelain veneers over 5 and 10 years. Int J Prosthodont. 2013; 26: 111-24.
Morimoto S, Albanesi RB, Sesma N, Agra CM, Braga MM. Main Clinical Outcomes of Feldspathic Porcelain and Glass-Ceramic Laminate Veneers: A Systematic Review and Meta-Analysis of Survival and Complication Rates. Int J Prosthodont. 2016; 29: 38-49.
Morimoto S, Rebello de Sampaio FB, Braga MM, Sesma N, Özcan M. Survival Rate of Resin and Ceramic Inlays, Onlays, and Overlays: A Systematic Review and Meta-analysis. J Dent Res. 2016; 95: 985-94.
Sjögren G, Bergman M, Molin M, Bessing C. A clinical examination of ceramic (Cerec) inlays. Acta Odontol Scand. 1992; 50: 171-8.
Pieger S, Salman A, Bidra AS. Clinical outcomes of lithium disilicate single crowns and partial fixed dental prostheses: a systematic review. J Prosthet Dent. 2014; 112: 22-30.
Näpänkangas R, Pihlaja J, Raustia A. Outcome of zirconia single crowns made by predoctoral dental students: a clinical retrospective study after 2 to 6 years of clinical service. J Prosthet Dent. 2015 Apr; 113(4): 289-94.
Tartaglia GM, Sidoti E, Sforza C. Seven-year prospective clinical study on zirconia-based single crowns and fixed dental prostheses. Clin Oral Investig. 2015; 19: 1137-45.
Passia N, Stampf S, Strub JR. Kassardjian. Five-year results of a prospective randomised controlled clinical trial of posterior computer-aided design-computer-aided manufacturing ZrSiO4 -ceramic crowns. J Oral Rehabil. 2013; 40: 609-17.
Larsson C, Wennerberg A. The clinical success of zirconia-based crowns: a systematic review. Int J Prosthodont. 2014; 27: 33-43.
Abdulmajeed AA, Donovan TE, Cooper LF, Walter R, Sulaiman TA. Fracture of layered zirconia restorations at 5 years: A dental laboratory survey. J Prosthet Dent. 2017; 118: 353-6.
Sulaiman TA, Abdulmajeed AA, Donovan TE, Cooper LF, Walter R. Fracture rate of monolithic zirconia restorations up to 5 years: A dental laboratory survey. J Prosthet Dent. 2016 Sep; 116(3): 436-9.
Pjetursson BE, Sailer I, Makarov NA, Zwahlen M, Thoma DS. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part II: Multiple-unit FDPs. Dent Mater. 2015; 31: 624-39.
Le M, Papia E, Larsson C. The clinical success of tooth- and implant-supported zirconia-based fixed dental prostheses. A systematic review. J Oral Rehabil. 2015; 42: 467-80.
Håff A, Löf H, Gunne J, Sjögren G. A retrospective evaluation of zirconia-fixed partial dentures in general practices: an up to 13-year study. Dent Mater. 2015; 31: 162-70.
Solá-Ruíz MF, Agustin-Panadero R, Fons-Font A, Labaig-Rueda C. A prospective evaluation of zirconia anterior partial fixed dental prostheses: Clinical results after seven years. J Prosthet Dent. 2015; 113: 578-84.
Rinke S, Wehle J, Schulz X, Bürgers R, Rödiger M. Prospective Evaluation of Posterior Fixed Zirconia Dental Prostheses: 10-Year Clinical Results. Int J Prosthodont. 2018; 31: 35-42.
Kern M, Passia N, Sasse M, Yazigi C. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J Dent. 2017; 65: 51-5.
Kern M, Sasse M. Ten-year survival of anterior all-ceramic resin-bonded fixed dental prostheses. J Adhes Dent. 2011; 13: 407-10.
Spitznagel FA, Horvath SD, Gierthmuehlen PC. Prosthetic protocols in implant-based oral rehabilitations: A systematic review on the clinical outcome of monolithic all-ceramic single- and multi-unit prostheses. Eur J Oral Implantol. 2017; 10 Suppl 1: 89-99.
Spies BC, Balmer M, Jung RE, Sailer I, Vach K, Kohal RJ. All-ceramic, bi-layered crowns supported by zirconia implants: Three-year results of a prospective multicenter study. J Dent. 2017; 67: 58-65.
Spies BC, Pieralli S, Vach K, Kohal RJ. CAD/CAM-fabricated ceramic implant-supported single crowns made from lithium disilicate: Final results of a 5-year prospective cohort study. Clin Implant Dent Relat Res. 2017; 19(5): 876-83.
Araujo NS, Moda MD, Silva EA, Zavanelli AC, Mazaro JV, Pellizzer EP. Survival of all-ceramic restorations after a minimum follow-up of five years: A systematic review. Quintessence Int. 2016; 47: 395-405.
Pihlaja J, Näpänkangas R, Raustia A. Early complications and short-term failures of zirconia single crowns and partial fixed dental prostheses. J Prosthet Dent. 2014 Oct; 112(4): 778-83.
Abou-Ayash S, Strasding M, Rücker G, Att W. Impact of prosthetic material on mid- and long-term outcome of dental implants supporting single crowns and fixed partial dentures: A systematic review and meta-analysis. Eur J Oral Implantol. 2017; 10 Suppl 1: 47-65.
Sailer I, Philpp A, Zembic A, Pjetursson BE, Hammerle CHF, Zwahlen M. A systematic review of the performance of ceramic and metal implant abutments supporting fixed implant reconstructions. Clin Oral Implants Res. 2009; 20(suppl 4): 4-31.
Hanh R, Weiger R, Netuschil L, Bruch M. Microbial accumulation and vitality on different restorative materials. Dent Mater. 1993; 9: 312-16.
Kawai K, Urano M. Adherence of plaque components to different restorative materials. Oper Dent. 2001; 26: 396-400.
Anusavice KJ, Phillips RW. Biocompatibility. In: Anusavice KJ, Shen C, Rawls HR, editors. Phillips' science of dental materials. 11th ed. St. Louis, Mo: Saunders; 2003. p. 111-47.
Lygre H. Prosthodontic biomaterials and adverse reactions: a critical review of the clinical and research literature Acta Odontol.Scand. 2002; 60: 1-9.
Thyssen JP, Menne T. Metal allergy-a review on exposures, penetration, genetics, prevalence, and clinical implications Chem.Res.Toxicol. 2010; 23: 309-18.
Burke F, Lucarotti P. Ten-year outcome of crowns placed within the general dental services in England and Wales. J Dent. 2009; 37: 12-24.
Scherrer S, Lohbauer U, Della Bona A et al. Adm guidance-ceramics: Guidance to the use of fractography in failure analysis of brittle materials. Dent Mater. 2017; 33: 599-620.
Pang Z, Chughtai A, Sailer I, Zhang Y. A fractographic study of clinically retrieved zirconia-ceramic and metal-ceramic fixed dental prostheses. Dent Mater. 2015; 31: 1198-1206.
Øilo M, Kvam K, Gjerdet N. Simulation of clinical fractures for three different all-ceramic crowns. Eur J Oral Sci. 2014; 122: 245-50.
Øilo M, Hardang A, Ulsund A, Gjerdet N. Fractographic features of glass-ceramic and zirconia-based dental restorations fractured during clinical function. Eur J Oral Sci. 2014; 122: 238-44.
Øilo M, Gjerdet N. Fractographic analysis of all-ceramic crowns: A study of 27 clinically-fractured crowns. Dent Mater. 2013; 29: e78-e84.
Quinn G, Hoffman K, Scherrer S et al. Fractographic analysis of broken dental restorations. Fractography of Glasses and Ceramics VI. Ceram Trans. 2012; 230: 161.174.
Lohbauer U, Amberger G, Quinn G.D, Scherrer S. Fractographic analysis of a dental zirconia framework: A case study on design issues. J Mech Behav Biomed Mater. 2010; 3: 623-9.
Aboushelib M, Salameh Z. Zirconia implant abutment fracture: Clinical case reports and precautions for use. Int J Prosthod. 2009; 22: 616-9.
Taskonak B, Yan J, Mecholsky Jr. J, Sertgöz A, Koçak A. Fractographic analyses of zirconia-based fixed partial dentures. Dent Mater. 2008; 24: 1077-82.
Moraguez O, Wiskott H, Scherrer S. Three- to nine-year survival estimates and fracture mechanisms of zirconia- and alumina-based restorations using standardized criteria to distinguish the severity of ceramic fractures. Clin Oral Investig. 2015; 19: 2295-307.
Pang Z, Chughtai A, Sailer I, Zhang Y. A fractographic study of clinically retrieved zirconia-ceramic and metal-ceramic fixed dental prostheses. Dent Mater. 2015; 31: 1198-206.
Du Q, Swain M, Zhao K. Fractographic analysis of anterior bilayered ceramic crowns that failed by veneer chipping. Quintessence Int. 2014; 45; 369-76.
Øilo M, Quinn G. Fracture origins in twenty-two dental alumina crowns. J Mech Behav Biomed Mater. 2016; 53: 93-103.
Kern M. Bonding to oxide ceramics-laboratory testing versus clinical outcome. Dent Mater. 2015; 31: 8-14.
Corresponding author: Ritva Näpänkangas, Research Unit of Oral Health Sciences, Faculty of Medicine, University of Oulu, P.O.Box 5281, FI-90014 University of Oulu, Finland. E-mail: ritva.napankangas@oulu.fiThis article has been submitted to peer reviews.Näpänkangas R, Larsson C, Øilo M. Clinical outcomes of ceramic restorations. Nor Tannlegeforen Tid. 2019; 129: 114-22
associate professor, DDS, PhD. Research Unit of Oral Health Sciences, Faculty of Medicine, University of Oulu, Finland
associate professor, DDS, PhD. Department of Materials Science and Technology, Faculty of Odontology, Malmö University, Sweden
Associate professor, DDS, PhD. Department of Clinical Dentistry, Faculty of Medicine, University of Bergen, Norway