Antibiotics in the treatment of periodontal and peri-implant infections
Adjunctive use of systemic antibiotics in the treatment of periodontitis and peri-implant infections has for many years been in focus for investigators due to the diversity in clinical picture and variability in treatment response in these conditions. Antimicrobial resistance has emerged as a serious problem worldwide and is one of the most important threats to global health as a result of misuse/overuse of antibiotics. Considering the diversity of the microbiota in the oral cavity and its potential to be a reservoir for antibiotic resistance genes, the misuse of antibiotics can result in negative effects for the individual and its surroundings. With the questionable positive long-term effect of antibiotics in most periodontal infections, use of antibiotics should be restricted and only considered after microbiological diagnostic testing that includes species identification and antibiotic susceptibility testing. For peri-implant infections, there is scarce evidence for the use of systemic antibiotics with no proven effective treatment protocol for good results on a long-term basis.
Headlines | |
|---|---|
· |
The microbiota in the oral cavity has the potential to act as a reservoir for antibiotic resistance genes. |
· |
The use of systemic antibiotics in the treatment of periodontal and peri-implant disease may thus be harmful for the ecosystems of the individual and its surroundings. |
· |
Considering the questionable positive and limited long-term effect in periodontal treatment, the use of systemic antibiotics should be restricted to aggressive periodontitis and/or unresponsive cases of advanced periodontitis. |
· |
Microbiological analysis including susceptibility testing are recommended in cases where antibiotics are considered as an adjunct to systematic periodontal treatment.« |
· |
The scientific evidence on the use of systemic antibiotics as an adjunctive treatment for peri-implantitis is scarce with no proven effective treatment protocol. |
This article will discuss the updated rationale for the supplementary use of systemic antibiotics (antibiotics administered per os) in periodontal and peri-implant infections in the light of the recent global antibiotic resistance threat. As a consequence, different aspects of clinical and microbiological considerations including relevant groups of antibiotics and their antimicrobial resistance, will be discussed. Aggressive and chronic periodontitis which comprise heterogeneous constellations of destructive periodontal disease, are included in the periodontitis section (1). The reader should be aware of the recently modified classification of periodontal diseases (2) where the two principal forms above have been put into the diagnosis «Periodontitis» (reclassified based on stages and grading). With the diverse clinical picture of periodontitis, the clinician will with either classification have to carefully evaluate each patient and decide an individual treatment plan. The general rule for adjunctive antibiotics must be restrictive, and the knowledge about the antibiotic resistance profile from microbiological testing is an important tool for a good treatment decision.
History of systemic antibiotics in periodontology
The basic approach for treatment of plaque-induced periodontitis has been established as anti-infective therapy; without the use of antibiotics (3 - 5). Long-term clinical studies have documented that infection control by mechanical periodontal treatment can be maintained with regular supportive care for most patients. The cornerstones in the maintenance are to monitor the quality of the patient´s oral hygiene, the clinical symptoms (bleeding on probing (BOP) and pocket probing depths (PPD) and X-ray information on a regular basis (6,7,8). Furthermore, periodontal therapy are dependent on skilled clinicians (dentists and dental hygients) who are able to diagnose and treat according to accepted guidelines (9).
Systemically administered antibiotics in this field was introduced in 1976 or even earlier when metronidazole was used for targeting anaerobic bacteria in dental infections (10). Tetracyclines were also tested experimentally (11 - 13) and used in cases of «juvenile periodontitis» (14), before amoxicillin or the combination of amoxicilin and metronidazole were shown to improve the treatment results (15,16). Later, studies by Loesche and coworkers showed a clinical benefit of metronidazole, used in addition to scaling and root planing (SRP), which seemed to reduce the need for periodontal surgery (17,18).
At the same time, Slots and coworkers reported on advanced cases of periodontitis where the treatment did not halt the periodontal breakdown. Such cases assigned as «refractory» or «therapy-resistant» may have originated from periodontal disease originally diagnosed as «chronic periodontitis». According to Armitage (9), «refractory periodontitis» could be a heterogenous group including multiple forms of nonresponsive periodontitis (19,20).
The observations of the periodontal microbiota «superinfected» with non-oral Gram negative facultative rods (Escherichia coli, Klebsiella pneumoniae, Serratia spp., Pseudomonas spp), yeasts, and even Staphylococcus aureus, often corresponded with these non-responsive cases. In vitro antibiotic resistance profiles to several antibiotics could also be detected as typical characteristics reflecting that the periodontal microbiota could be a reservoir of bacterial resistance. More than 20 years later, data from microbiological samples of untreated periodontitis patients show a high prevalence of antibiotic resistance in the microbiota, supporting its role as a reservoir of antibiotic resistance genes (21,22).
Periodontitis
Aggressive periodontitis and chronic periodontitis
In the classification from 1999 «juvenile periodontitis» was placed in the aggressive periodontitis group (1) due to characteristics with early onset and rapid attachment loss. Treatment of these cases have for many years been accepted as a challenge for the clinician. If treatment is to succeed tooth loss should be limited as much as possible and be intensive and careful with the clinician's knowledge of etiology, pathogenesis, microbiology and clinical features. Patients included in these categories are those who may benefit from the use of systemic antibiotics as a supplement to conventional periodontal treatment (16,23). However, antibiotics should only be prescribed to patients with severe periodontal breakdown in order to treat the patients individually and reduce antibiotic use to the minimum.
Localized and generalized aggressive periodontitis have several common clinical characteristics, including a 3 - 4 fold higher speed of progression/destruction rate compared to chronic periodontitis (1,24). Periods of progression are followed by periods of regression (25). The treatment should always include an initial periodontal therapy phase, a second phase that may include the use of antibiotics together with SRP or SRP plus periodontal surgery, with a carefully planned supportive therapy (maintenance) in all cases. Since the biofilm is 100 - 1000 times more resistant to antibiotics than planktonic bacterial cells (26, 27), the biofilm must be broken mechanically to make the antibiotics sufficiently effective in reaching the target.
The rationale for the use of antibiotics is that pathogens after mechanical debridement persist in the periodontal tissue, in furcation involvements, root concavities or dentin tubules and may recolonize as the basis for recurrent disease. The presence of Aggregatibacter actinomycetemcomitans and Porphyromonas gingivalis in the microbiota in patients with aggressive periodontitis may have increased indication for the use of supplementary antibiotics due to their ability to invade host tissue cells (epithelial and connective tissue cells) (28,29). If antibiotics are to be prescribed, it should be administered during a short period of disease activity/progression, and considered only for patients with sufficient oral hygiene (plaque index not exceeding 15 %) after initial treatment. These criteria for antibiotics should be met: Presence of several probable pockets of ? 6mm (at least 2 sites in patients with localized aggressive periodontitis), persistent inflammation registered as BOP and/or suppuration, increased loss of attachment, verified progression of bone loss on radiographs and an unfavorable subgingival microbiota (30). Thus, the adjunctive use of antibiotics in patients with aggressive periodontitis has become part of the national antibiotic guidelines in several countries due to the reported effect of systemic antibiotic therapy with a mean difference in PPD and CAL of 1.05 mm and 1.08 mm 6-month post-treatment, respectively (31,32).
If antibiotics are considered in the treatment of periodontits, it should always be administered as a supplement to conventional therapy (27,33).
Many studies with variable observation periods and results have during the last twenty years been performed to evaluate the effect of adjunctive systemic antibiotics as part of the initial treatment of chronic periodontitis. Several treatment schemes have been used followed by discussions and arguments of pro et contra of how to implement these drugs with the best effect, and several types of antibiotics have also been tested. Most prevalent is the combination of amoxicillin and metronidazole (34).
According to a meta-analysis from 2003 analyzing 29 studies, the authors (33) concluded that systemic antibiotics had a statistically significant positive effect on clinical attachment loss with the greatest effect in patients with aggressive periodontitis compared to those with chronic periodontitis. This study, other systematic reviews and meta-analyses of non-surgical periodontal therapy supplemented with systemic antibiotics in patients with untreated chronic periodontitis (35) indicate only a minimal clinical measurable effect in previously untreated patients. In earlier studies, patients with chronic periodontitis responded well to mechanical debridement when the oral hygiene was sufficient, and the disease was diagnosed in time (36 - 38). Recent studies support that there was no significant long-term effect after 5 years on PPD, CAL or tooth loss when metronidazole was used alone as a supplement to SRP (39,40).
Peri-implantitis
The inflammatory process, potentially leading to destruction of the supportive bone around osseointegrated dental implants, is also related to formation of oral biofilms on inert implant surfaces (41). Therefore, a personalized oral hygiene protocol and controlled maintenance care intervals after implantation are crucial in the primary prevention of peri-implant diseases (42 - 44). The wide variation in prevalence of peri-implantitis in several reports may be explained by different criteria for the amount of alveolar bone loss defined as pathological and for the follow-up time of implants in function. Since there is an increasing trend to use dental implants to replace missing teeth instead of conventional prosthodontic reconstructions, there will be a continuous need for efficient treatment options for peri-implant diseases, especially peri-implantitis. It has been estimated that more than 12 million implants are placed globally every year (45). At patient level, a meta-analysis presented weighted mean values of 42.9 % for peri-implant mucositis and of 21.7 % for peri-implantitis (46). In Sweden, it was recently shown that during a time period of nine years, 14.5 % of the patients treated with dental implants developed a moderate to severe form of peri-implantitis (47).
Periodontitis versus peri-implantitis - similar or different?
Periodontitis and peri-implantitis are both infections linked to the formation of biofilms located at the gingival margin where the subgingival/submucosal sites of an affected tooth/implant have similar major risk factors, such as poor oral hygiene, smoking, and diabetes (43,48,49). Periodontitis per se forms an increased risk for peri-implantitis (48,49,50). One drastic difference is a non-linear, accelerating pattern of bone destruction and its fast progression in peri-implantitis (51,52). In addition, the type of implant surface seems to have an impact on the susceptibility to develop peri-implantitis and on the resolution of infection (53,54).
The periodontal pathogens have been considered causative agents also in peri-implantitis due to the potential transmission of pathogenic species from periodontal pockets to peri-implant sites (55,56). Factors that determine the compostion of the periodontal microbiota are defined by the microbial ecological niche (57). Essential for subgingival bacterial growth is the anaerobic conditions, the supply of nutrients from the gingival crevicular fluid, temperature and other factors which favor the composition of the microbiota in that niche.
The microbiota of chronic periodontitis has been characterized by different bacterial complexes that cooperate in the pathogenesis (58). The red complex consists of Porphyromonas gingivalis, Tannerella forsythia and Treponema denticola and with the members of the orange complex (a number of other anaerobic, Gram negative species) have been proposed to be responsible for disease progression (figure 1). The established subgingival biofilm in periodontitis is dominated by facultative and strict anaerobic species including Prevotella spp., Fusobacterium spp. Porphyromonas spp.; Treponema spp. and others. Recent studies indicate that Porphyromonas gingivalis represents a «keystone pathogen» which is able to modulate the subgingival biofilm into dysbiosis, thus exerting the whole bacterial community into disfavor of the host (59,60). A. actinomycetemcomitans associated with local aggressive periodontitis («juvenile periodontitis») may also be detected in other forms of periodontal disease. Thus, the virulence factors of these species represent a potential arsenal for local tissue destruction.
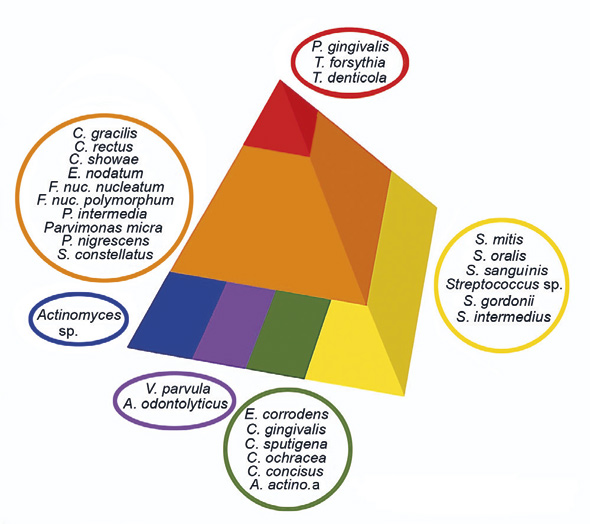
Figure 1. Bacterial complexes in chronic periodontitis. The red and orange complexes are associated with the cultivable species in the microbiota important in the pathogenesis of chronic periodontitis. From Socransky et al.,1998.
The red complex bacteria (Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia) are abundant in peri-implantitis as well. Microbial interacting networks are dissimilar between periodontitis and peri-implantitis (61). In a study by Kumar and coworkers (62), significant compositional differences were detected between four groups with healthy teeth, teeth with periodontitis, healthy implants or implants with peri-implantitis. The bacterial communities varied considerably between teeth and implants in health and between periodontitis and peri-implantitis samples. Interestingly, peri-implant communities proved to be less diverse, and several species, including previously unsuspected and unknown organisms, were unique to the peri-implant niche (62). These results also correspond with results from earlier studies indicating a similarity with cases of «refractory» or «therapy-resistant periodontitis» (non-oral Gram negative rods, pseudomonads and S. aureus and with detectable in vitro resistance to several antibiotics).
The bacterial profiles in peri-implant health and disease have been summarized in recent systematic reviews (63, 64).
Results from new advancements in gene sequencing methods have also revealed the microbial diversity in peri-implant sites. In different studies, peri-implant biofilms are reported to contain known periodontitis-associated species and opportunistic pathogens (53,65), to be connected to periodontal pathogens and staphylococci (62,66,67). In addition, certain clusters of spirochetes (Treponema) and Synergistetes, which are mainly uncultivable, have been observed in increased prevalence and numbers in peri-implantitis lesions (68). Some reports also indicate that viruses (Epstein-Barr virus-1 and human cytomegalovirus-2) may contribute to the pathogenesis (69), as has been proposed for periodontitis (70).
To date, there is increasing evidence on the effect of smoking on the composition of subgingival biofilms. It seems that smoking shapes the peri-implant microbiome even during clinical health by depleting commensals and enriching for pathogens (71). In both smokers and non-smokers, peri-implant mucositis is a sentinel event indicating the environment is primed for future disease.
There is evidence that diabetes is linked to changes in the periodontal/peri-implant microbiota. Demmer and co-workers investigated abnormal glucose metabolism and periodontal microbiota prior to diabetes development and overt hyperglycemia; higher levels of many subgingival bacteria associated with a two- to three-fold higher prevalence of prediabetes among diabetes-free adults (72). A study by Ganesan and co-workers (2017) revealed that environmental stress, caused by smoking and diabetes, affects the structure and membership of the subgingival microbial communities. The combined effect of smoking and hyperglycemia proved to be greater than the sum of the parts (73). It was shown that a hyperglycemic microenvironment favors organisms that thrive under glucose-rich, pro-oxidant, protein-rich, and anaerobic conditions. No such data exist on dental implant-related submucosal biofilms so far. However, in a recent systematic review, it was demonstrated that hyperglycemic individuals have an increased risk for peri-implantitis but not for peri-implant mucositis (74).
Antimicrobial resistance (AMR)
Most of the studies in periodontal literature investigating the effect of adjunctive use of antibiotics are primarily focusing on the clinical effect of the treatment and do not take into account the negative side-effects of these drugs: 1) the questionable and unethical use of broad spectrum antibiotics with no actual information about the microbiota (composition and resistance profile (see later), 2) the negative effects on the normal microbiota (unfavorable dysbiosis in the gut and other niches), and 3) the upgrowth of resistant bacterial clones. Investigations demonstrating these side effects have been available for many years, but may have been forgotten in the context of the goal of a successful periodontal treatment. Now, it is time to closer elucidate and weigh the pro et contras for adjuntive antibiotics in periodontology (21, 23,75). These are are summarized in figure 2.
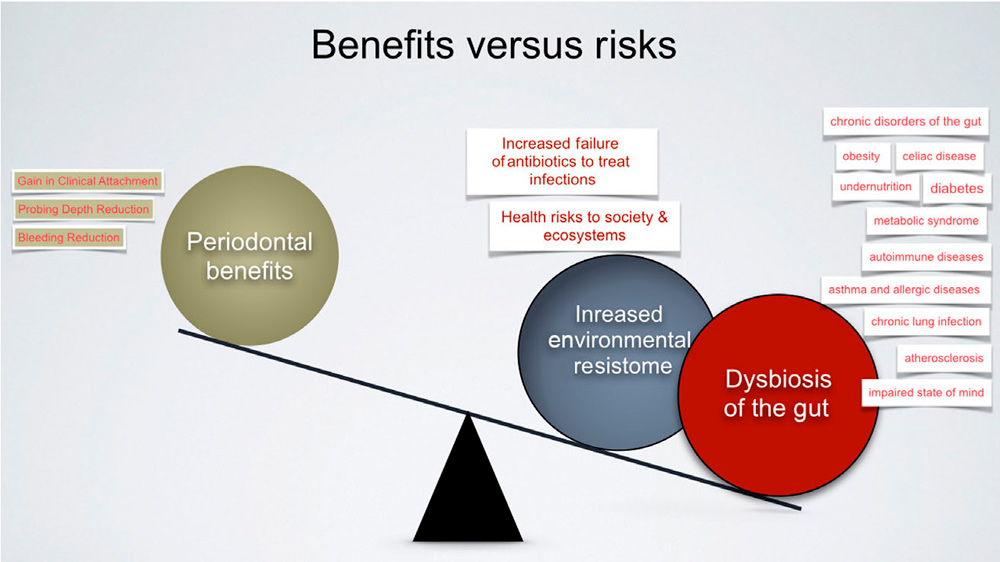
Figure 2. Benefits of systemic antibiotics as an adjunct in the treatment of periodontitis versus the health risks to society and the worlds´s ecosystems. From Jepsen and Jepsen, 2016 (Courtesy: G. Armitage).
AMR is the ability of bacteria to survive and grow in the presence of antimicrobial drugs. It is a natural phenomenon that existed long before the introduction of antibiotics in medicine and can be an intrinsic property of a species, which means that all members of the species are resistant to a certain compound. It is however important to realize that AMR is an emerging problem worldwide and according to the WHO, one of the most important threats to global health (76, 77). This is associated with the potential of susceptible microorganisms to acquire resistance to drugs. The emerging problem with spread of AMR in previously susceptible species directly which is connected with the overuse and misuse in human and veterinary medicine and food production (78). Bacteria can acquire AMR by either mutation of existing genetic material that changes or enhances the activity of a gene product or horizontal gene transfer (HGT) of extrinsic DNA creating novel genetic material. Horizontal gene transfer occurs via three general mechanisms: 1) phage transduction, 2) transformation and 3) conjugation. Phage transduction is the transfer of genetic material via infection by a bacterial virus - a bacteriophage (79). Transformation is the acquisition of extracellular genetic material from the environment whereas conjugation is direct cell-to-cell transfer of genetic material via conjugative pili.
Antimicrobial drugs generally target one of the essential structures or processes of bacteria including the cell membrane or enzymes involved in: i) maintenance of the cell wall, ii) replication, iii) transcription, iv) translation or v) metabolism. The mechanisms utilized by bacteria to withstand the effect of antimicrobial drugs are generally divided into three major strategies: 1) prevention of the drug from reaching its target, 2) alteration of the target or 3) inactivation of the drug (80).
Antimicrobial drugs can be prevented from reaching the intended target by passive mechanisms such as the natural barriers that exist in certain types of bacteria such as the outer membrane of Gram negative bacteria. Both Gram positive and Gram negative bacteria also possess membrane spanning proteins (efflux pumps) that actively extrude drugs from the cytoplasm thereby reducing the intracellular concentration. There are both specific and multi-drug transporters, with affinity for one or different types of drugs, respectively. Protection of the target site can also often be achieved by expression of specific proteins that interact with the drug target and prevent access of the drug to the target site. A common strategy of bacteria to resist antimicrobial activity is to alter the target which may reduce the interaction between the drug and target. These modifications can consist of point mutations in the genes encoding the target, enzymatic alteration of the drug binding site or replacement or bypass of the original target. Inactivation of the antimicrobial drugs occurs via enzyme mediated chemical modifications, such as acetylation, phosphorylation, adenylation or hydrolysis of essential components of the drugs. This leads to reduced binding to the target or destruction of the drug (80). Importantly, resistance mechanisms against several antibiotics often localize on the same transferrable genetic element, which means that the use of one class of antibiotics may promote persistence and spread of resistance mechanisms to other classes of antibiotics, hence increasing the dissemination of multidrug resistant bacteria (81).
Microbial diagnostics in periodontits and peri-implantitis
Bacterial sampling from periodontitis and peri-implant sites can be performed either with sterile paper points, a sterile periodontal probe or a curette. Since it is easy to induce bleeding from initially inflamed deep pockets, paper points are usually preferred to minimize the risk of blood contamination. Samples are usually taken for analysis with DNA probes (checkerboard) or with PCR (qPCR/or real time PCR) (82) and transported dry, in a buffer solution or in an anaerobic transport medium to the laboratory. The choice of transport medium for transfer of viable anaerobic bacterial samples is of outmost importance for the culture analysis because invitro susceptibility testing can only be performed when the bacterial samples contain viable bacteria (83).
As a general molecular screening of periodontitis or peri-implant microbiota, the DNA checkerboard analysis has been used for many years and represents a panel of predefined DNA probes (bacterial markers) where many samples can be tested at the same time (84). Analysis with qPCR has a greater sensitivity but is limited by the fact that fewer bacterial species (red complex) can be routinely quantified. In addition to identification by molecular methods, cultivation and susceptibility testing should always be included in the total microbial analysis due to the increasing antibiotic resistance that has emerged (see below). For cultivation, both anaerobic and aerobic conditions ought to be included as well as detection of superinfecting organisms such as enteric rods and Candida spp. by using selective agar media for these organisms. The susceptibility testing should include antibiotics and antifungal medicaments that are used in dental infections.
Need for antibiotic susceptibility testing
Since there is a direct correlation between antibiotic consumption and the global development of resistance (85,86), every effort has to be taken to reduce antibiotic misuse/overuse. A serious problem with the development of oral bacterial resistance is that the commensal bacteria also may transfer resistance genes to other pathogens such as Streptococcus pyogenes (87), supporting that the oral microbiota can be reservoir of AMR. Rams and co-workers (88) found that 71.7 % of 120 peri-implantitis subjects exhibited submucosal bacterial pathogens resistant in vitro to one or more of the tested antibiotics (doxycycline, clindamycin, amoxicillin, and metronidazole) (see earlier, (21)).
For targeted selection of adjunctive antibiotic treatment, it would be of outmost importance to test the antibiotic susceptibility pattern in periodontitis and peri-implant infections. Susceptibility testing of relevant microorganisms is performed at most microbiological laboratories. However, unless these laboratories have special knowledge and interest in the «niche» of oral microbiology, important details in the analysis may easily be overlooked. Bacterial susceptibility testing against antibiotics used in dental care should be preferred, but there is no consensus on how the oral microbial analysis should be designed. Under any circumstance, in vitro antibiotic susceptibility testing should always be included in the microbial analysis to be of any value in the clinic (89). Even in the Scandinavian countries, a coordination of these matters should be focused on.
For peri-implantitis, it seems that the benefits of the adjunctive use of antibiotics in the treatment remain questionable. Whenever prescribing antibiotics, it is important that clinicians carefully consider expected benefits and risks, including side effects due to disturbance of the commensal flora in the gut, and in particular, the risk of the development of resistant clones. Peri-implant superinfections form a potential risk in patients treated empirically with broad-spectrum antibiotics (90). Gastrointestinal discomfort and mild diarrhea seem to occur in approximately 10 % of the cases treated with a single antibiotic(54,91), whereas side effects are more common when the combination of amoxicillin and metronidazole is used (92).
Antibiotic resistance mechanisms
Beta-lactam resistance
Phenoxymethylpenicillin and amoxicillin are ?-lactam antibiotics commonly used in dentistry. This class of bactericidal drugs function by inhibiting the transpeptidase reaction catalyzed by penicillin binding proteins (PBP) during synthesis of the peptidoglycan layer of the bacterial cell wall. The result is a weak cell wall and cells that easily burst due to osmotic lysis (93). Because of physiological differences between Gram positive and Gram negative bacteria and differences in number, activity and functionality of PBP of different species, bacterial species are differently susceptible to various ?-lactam antibiotics (94,95,96).
The most important mechanism of resistance to ?-lactam antibiotics is the enzyme mediated hydrolysis of the ?-lactam ring, resulting in inactivation of the drug. These enzymes are called ?-lactamases and are strategically located together with the PBP; extracellularly in Gram positive bacteria and in the periplasmic space of Gram negative bacteria (93). In this way they protect the integrity of the peptidoglycan layer by inactivating the antibiotic before it can inhibit the transpeptidase activity of the PBP and weaken the cell wall. They are naturally occurring and chromosomally encoded in many species, but can also occur in mobile genetic elements including integrons and plasmids, which facilitate their dissemination.
Bacteria can be intrinsically resistant to some ?-lactam antibiotics due to differences in the structure of PBP. Resistance also occurs due to mutations in genes encoding PBP that result in structural changes and altered affinity for the antibiotic. This has been described for methicillin resistant Staphylococci (MRSA) (97) as well as penicillin resistant Streptococci and Neisseria species (98,99).
Because of the occurrence of penicillin resistance, novel ?-lactam antibiotics were developed to circumvent the problem. However in parallel, novel ?-lactamases with wider spectrum of activity emerged and/or spread in bacterial communities counteracting the development of new generations of drugs. This explains the complex and intriguing problem of AMR where the bacteria always find a new way to survive by genetic modification and exchange.
The extended spectrum ?-lactamases (ESBL) are enzymes that can inactivate 3rd generation cephalosporins as well as earlier generation drugs (100). Dissemination of plasmid encoded extended spectrum ?-lactamases is an emerging problem because they are resistant to most ?-lactam antibiotics, and in addition, these plasmids often contain resistance mechanisms against other antibiotics leaving very few treatment options available (101). The treatment of choice for serious infections caused by ESBL producing organisms is carbapenem, but plasmid mediated carbapenem-resistance has recently been described (102). Carbapenem resistant organisms are classified as priority 1: critical in need of development of novel antibiotics by the world health organization (103).
Clindamycine resistance
Clindamycin is a semisynthetic antibiotic of the lincosamide family, with primarily bacteriostatic effect. It is mainly active against Gram positive bacteria, and anaerobic bacteria (104), and thus could be excellent for the treatment of odontogenic infections, including periodontal and peri-implant infections. It binds to the 50S ribosomal subunit and inhibits bacterial protein synthesis by interfering with the transpeptidation reaction and peptide-chain elongation (105). The drug shows little effect against most aerobic Gram negative bacteria due to their intrinsic resistance and poor permeability of the cellular outer porins (104).
However, there are several mechanisms of resistance to clindamycin, including modification of the target, inactivation of the drug and drug efflux (104,105). Resistance occurs by both plasmid mediated and chromosomally mediated mechanisms and include chromosomal mutations of ribosomal subunits, plasmid encoded efflux pumps and drug-adenylating or ribosome-methylating enzymes altering the drug-ribosome interaction. Thus, the drugs ability to counteract antibiotics and cause AMR by several different mechanisms should be taken as a warning by the clinicians intending to use it, and it constitutes an example of the importance of susceptibility testing in the microbial analysis.
Metronidazole resistance
For some clinically important anaerobic species a slight increase in resistance to metronidazole has been reported, but fragmented information is available (106,107). Metronidazole belongs to the nitroimidazole group and is mainly active against obligate anaerobic bacteria (and to a small extent microaerophilic or facultative anaerobes), while Actinomyces and Propionebacterium spp. are resistant (108). This indicates that the metabolic state of the organism is important and in line with the fact that the drug must be reduced to be active (109). The ability of metronidazole to compete as an electron acceptor is important for function and changes in metabolism of organisms have been shown to impact the susceptibility to metronidazole. The mechanisms of resistance are complex and includes reduced uptake, increased efflux, reduced rate of drug activation, drug inactivation and increased DNA repair mechanisms (21,109), with only scarce information available.
Quinolone resistance
Ciprofloxacin is one of the drugs in the group of fluoroquinolones. The drug targets are the type II topoisomerases gyrase and topoisomerase IV (110). These drugs are ineffective in anaerobic infections, while effective to non-oral Gram negative rods (E. coli, Klebsiella spp., Pseudomonas spp. etc.) frequently detected in therapy-resistant periodontal and in peri-implant infections. Acquired quinolone resistance is associated with three types of mechanisms: i) chromosomal mutations altering the drug binding affinity, ii) chromosomal mutations resulting in decreased influx or increased efflux of the drug and iii) acquisition of plasmid mediated genes coding for target protection proteins, drug modifying enzymes or drug efflux pumps (111). The quinolones are extreme drivers of antibacterial resistance, and for the use of quinolones in this respect, susceptibility testing and careful consideration about all aspects of the patient is of outmost importance (112).
Quinolone resistance can occur as a result of decreased influx, increased efflux or both. Exposure of bacteria to quinolones can select for mutants that overexpress efflux pumps, usually as a result of mutations in regulatory proteins and less often as a result of mutations in the structural genes associated with quinolone resistance. In general mutations affecting quinolone uptake and efflux cause only low-level resistance and do not usually represent a major clinical problem in the absence of additional resistance mechanisms (110, 111, 112). However, efflux systems have been shown to be of critical importance for the development of high level quinolone resistance and reduced intracellular concentration of quinolones may favour the emergence and dissemination of other types of resistance. Efflux pumps involved in quinolone resistance have been identified in both Gram positive and Gram negative species.
Tetracycline resistance
Tetracyclin is a broad spectrum antibiotic that interacts with the 16S rRNA of the 30S ribosomal subunit, thereby inhibiting protein synthesis by blocking attachment of charged aminoacyl-tRNA to the A site of the ribosome (113,114). Tetracycline enters Gram negative cells via diffusion through the outer membrane porins. Resistance to tetracyclines often occur as a result of acquisition of mobile genetic elements carrying tetracycline resistance determinants, mutations within the ribosomal genes or mutations leading to decreased cytoplasmic accumulation of the drug (115).
Macrolides
Macrolide antibiotics are natural or semisythetic compounds that function by binding to the ribosome and stalling protein synthesis (116). Macrolide resistance are increasing and can occur via several different mechanisms. The use of macrolides has been shown to induce mutations in the chromosomally encoded 23S ribosomal RNA (rRNA) as well as in genes encoding protein subunits of the ribosome (117). The rRNA methyl transferases constitute an important and widespread resistance mechanism that function by methylating a residue in the 23S rRNA and thereby prevent interaction between the ribosome (target) and the macrolide drug (118,119). Mutations and/or methylation of rRNA or ribosomal protein subunits separately lead to reduced macrolide susceptibility and can in combination result in high level of macrolide resistance (120,121). Importantly, the binding site of macrolides, lincosamides and streptogramins overlap, and it has been shown that mutations or methylation of the rRNA can confer cross-resistance to drugs of these three antibiotic classes and expression of the MLSB-phenotypes (varying levels of Macrolide, Lincosamide, Streptogramin B resistance) (122). Furthermore, macrolide can be inactivated by macrolide esterases and/or phosphotransferases that hydrolyze macrolides or transfer a phosphate moiety onto the drug (123,124). There are both specific macrolide efflux pumps and unspecific multidrug resistance pumps that can lower the intracellular concentration of macrolides in both Gram positive and Gram negative bacteria (117).
Treatment
Treatment of aggressive and refractory periodontitis with adjunctive antibiotics
The most commonly used systemic antibiotics are metronidazole, amoxicillin and tetracycline /doxycycline. Amoxicillin has a broad antimicrobial spectrum and is bactericidal on Gram-positive cocci and rods, Gram-negative cocci and some Gram-negative rods. Metronidazole primarily inhibits strict anaerobe microorganisms, and in combination with amoxicilline has a synergistic effect on the facultative part of the microbiota, including A. actinomycetemcomitans (A.a) (125). Due to the relatively high occurrence of A.a. in patients with localized aggressive periodontitis, the combination of these two drugs is the primary choice. In cases of ?-lactamase producing organisms amoxicillin plus + clavulanic acid (?-lactamase inhibitor) will be a preference if it is available for prescription in the primary care.
Tetracycline/doxycycline, a broad spectrum antibiotic from the TET-group, is less effective against periodontal infections with A.a. However, due to a high degree of bacterial resistance, the use of these drugs should be minimized as much as possible (126). Doxycycline can be administered if its anti-collagenase effect is considered important (127).
Microbiological testing of the subgingival microbiota including identification and susceptibility testing to appropriate antibiotics should always be performed for the use of broad spectrum antibiotics proposed in the treatment of periodontal infections due to the fact that the clinical picture cannot display species identification or susceptibility pattern of the microbiota of interest.
The final decision on the use of antibiotics must be based on anamnestic information on health status and previous periodontal treatment, clinical parameters, radiographic analysis of bone loss and infrabony defect formation.
Treatment of peri-implantitis with adjunctive antibiotics
In the treatment of advanced peri-implantitis, mechanical anti-infective therapy is necessary but seldom results in the resolution of the infection, and therefore, access surgery is considered an essential part of the treatment (128). Systemic antibiotics have been used both in the mechanical anti-infective treatment phase and in connection to regenerative surgical procedures. However, no standardized guidelines are available regarding the use of systemic antibiotics in peri-implantitis. Adjunctive antimicrobials have been advised as a potential treatment regimen in severe cases, like in those having deepened pockets of >5 mm, notable cratering of more than 2 mm, and bleeding on probing, as stated in the cumulative interceptive supportive therapy (CIST) flowchart (129).
There are studies where systemic antimicrobials and antiseptics are routinely included in the surgical treatment protocol of peri-implantitis. In a two year prospective study, all 31 patients started a prophylactic one week course of clindamycin the day before surgery (130). A delay of re-growth of submucosal bacteria at the 6-month examination did not sustain, where only 50 % of the patients were without signs of peri-implant disease after two years. A study from Switzerland and Western Australia including 24 patients treated with a combination of amoxicillin and metronidazole (seven days), starting immediately after surgery, showed that the majority of peri-implantitis patients can be treated successfully, with a strict anti-infective protocol (5). In a five year follow-up of these patients with regularly supportive peri-implant therapy, 63 % had a successful treatment outcome (53 % at implant level) (131). An anti-infective surgical peri-implantitis treatment protocol with adjunctive antimicrobials and regular maintenance visits was considered moderately effective. Thus, it is not possible to solve the role of antibiotics as a separate issue in the treatment outcome, since randomized controlled clinical trials are needed to show the effect of selected adjunctive systemic antimicrobials.
One randomized controlled clinical trial, where 100 patients with 179 dental implants affected by severe peri-implantitis were recruited to investigate the adjunctive effect of systemic antibiotics (amoxicillin) and local antimicrobial decontamination agents (chlorhexidine) (54). The patients were randomly assigned to four groups, of those two groups with or without antimicrobial decontamination, and they had a ten day course of amoxicillin, commenced three days prior to resective surgery. One fourth of the implants had a non-modified surface, while the rest presented different types of modified surfaces. The microbiological and clinical treatment outcome was evaluated at six- and 12-month intervals; while bone gain was reported in patients treated with adjunctive amoxicillin and further bone loss was observed in those without amoxicillin. Interestingly, only a minor positive effect was found around implants with non-modified surface, whereas the potential benefit of systemic amoxicillin was limited to implants with modified surfaces (54). In a subsequent 3-year follow-up, the analysis included 83 patients and 148 implants, confirming the positive outcome of surgical therapy for the majority of these peri-implantitis patients (132). Whether surface characteristics influence long-term treatment outcomes and the susceptibility to recurrent disease could be speculated, because the pocket depth reduction was more pronounced at implants with non-modified surface. Instead, the moderate benefit of systemic amoxicillin that was gained at implants with modified surfaces at the time of first intervention (54) did not sustain over the follow-up period of three years (132).
Azithromycin belongs to newer macrolides, and it is increasingly used in periodontics. It has been shown to be able to suppress periodontal pathogens, to possess anti-inflammatory properties, and to persist in host cells like gingival fibroblasts and macrophages (133). However, the reported short-term effect of azithromycin at clinical and microbiological level does not support its use in the treatment of peri-implantitis (91, 134) (see also section Antibiotic resistance mechanisms).
Conclusions
The scientific evidence for the benefits of adjunctive systemic antibiotics in the treatment of periodontitis and peri-implantitis are generally not acceptable due to the unfavorable health risks to patients, society and the worlds´s ecosystems. However, in cases of aggressive and unresponsive cases of advanced chronic periodontitis antibiotics could be considered after microbiological analysis based on molecular methods, culture analysis (anaerobic and aerobic growth) and susceptibility testing.
Reliable scientific evidence on the use of systemic antimicrobials as an adjunctive treatment for peri-implantitis is scarce with no proven effective treatment protocol to keep all peri-implantitis patients free of inflammation on a long-term basis, underlining the significance of preventive approach for individuals with dental implants.
References
Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999 Dec; 4(1): 1 - 6.
Caton J, Armitage G, Berglundh T, Chapple I, Jepsen S, Kornman K, Mealey B, Papapanou PN, Sanz M, Tonetti, M. A new classification scheme for periodontal and peri-implant diseases and conditions -Introduction and key changes from the 1999 classification. J Clin Periodontol. 2018; 45: 45 (Suppl 20) S1 - 8.
Socransky SS. Microbiology of periodontal disease - present status and future considerations. J Periodontol. 1977 Sep; 48(9): 497 - 504.
Socransky SS, Haffajee AD. The bacterial etiology of destructive periodontal disease: current concepts. J Periodontol. 1992 Apr; 63(4 Suppl): 322 - 31.
Heitz-Mayfield LJ, Lang NP. Surgical and nonsurgical periodontal therapy. Learned and unlearned concepts. Periodontol 2000. 2013 Jun; 62(1): 218 - 31.
Axelsson P, Lindhe J. The significance of maintenance care in the treatment of periodontal disease. J Clin Periodontol. 1981 Aug; 8(4): 281 - 94.
Moser P1, Hammerle CH, Lang NP, Schlegel-Bregenzer B, Persson R. Maintenance of periodontal attachment levels in prosthetically treated patients with gingivitis or moderate chronic periodontitis 5 - 17 years post therapy. J Clin Periodontol. 2002 Jun; 29 (6): 531 - 9.
Axelsson P, Nyström B, Lindhe J. The long-term effect of a plaque control program on tooth mortality, caries and periodontal disease in adults. Results after 30 years of maintenance. J Clin Periodontol. 2004 Sep; 31(9): 749 - 57.
Armitage GC. Periodontal diagnoses and classification of periodontal diseases. Periodontol 2000. 2004; 34: 9 - 21.
Loesche WJ. Chemotherapy of dental plaque infections. Oral Sci Rev. 1976; 9: 65 - 107.
Listgarten MA, Lindhe J, Hellden L. Effect of tetracycline and/or scaling on human periodontal disease. Clinical, microbiological, and histological observations. J Clin Periodontol. 1978 Nov; 5(4): 246 - 71.
Helldén LB, Listgarten MA, Lindhe J. The effect of tetracycline and/or scaling on human periodontal disease. 1979 Aug; 6(4): 222 - 30.
Lindhe J, Liljenberg B, Adielsson B. Effect of long-term tetracycline therapy on human periodontal disease. J Clin Periodontol. 1983 Nov; 10(6): 590 - 601.
Slots J, Rosling BG. Suppression of the periodontopathic microflora in localized juvenile periodontitis by systemic tetracycline. J Clin Periodontol. 1983 Sep; 10(5): 465 - 86.
van Winkelhoff AJ, Rodenburg JP, Goené RJ, Abbas F, Winkel EG,de Graaff J. Metronidazole plus amoxycillin in the treatment of Actinobacillus actinomycetemcomitans associated periodontitis. J Clin Periodontol. 1989 Feb; 16(2): 128 - 31.
Keestra JA, Grosjean I, Coucke W, Quirynen M, Teughels W. Non-surgical periodontal therapy with systemic antibiotics in patients with untreated aggressive periodontitis: a systematic review and meta-analysis. J Periodontal Res. 2015 Dec; 50(6): 689 - 706.
Loesche WJ, Giordano JR, Hujoel P, Schwarcz J, Smith BA. Metronidazol in periodontitis: reduced need for surgery. J Clin Periodontol. 1992; 19: 103 - 12.
Loesche WJ, Giordano J, Soehren S, Hutchinson R, Rau CF, Walsh L, Schork MA. Nonsurgical treatment of patients with periodontal disease. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996 May; 81(5): 533 - 43.
Slots J, Rams TE. New views on periodontal microbiota in special patient categories. J Clin Periodontol. 1991 Jul; 18(6): 411 - 20.
Colombo AP, Haffajee AD, Dewhirst FE, Paster BJ, Smith CM, Cugini MA, Socransky SS. Clinical and microbiological features of refractory periodontitis subjects. J Clin Periodontol. 1998 Feb; 25(2): 169 - 80.
Rams TE, Degener JE, van Winkelhoff AJ. Antibiotic resistance in human chronic periodontitis microbiota. J Periodontol. 2014 Jan; 85(1): 160 - 9.
van Winkelhoff AJ, Rurenga P, Wekema-Mulder GJ, Singadji ZM, Rams TE. Non-oral gram-negative facultative rods in chronic periodontitis microbiota. Microb Pathog. 2016 May; 94: 117 - 22.
Jepsen K, Jepsen S. Antibiotics/antimicrobials: systemic and local administration in the therapy of mild to moderately advanced periodontitis. Periodontol 2000. 2016 Jun; 71(1): 82 - 112.
Baer PN. The case for periodontosis as a clinical entity. J Periodontol. 1971; 42: 516 - 20.
Goodson JM, Tanner ACR, Haffajee AD, Sornberger GC, Socransky SS. 2007. Patterns of progression and regression of advanced destructive periodontal disease: J Clin Periodontol. 1982; 9: 472 - 81.
Sedlacek MJ, Walker C. Antibiotic resistance in an in vitro subgingival biofilm model. Oral Microbial Immunol. 2007; 22: 333 - 9.
Herrera D, Alonso B, León R, Roldán S, Sanz M. Antimicrobial therapy in periodontitis: the use of systemic antimicrobials against the subgingival biofilm. J Clin Periodontol. 2008 Sep; 35(8 Suppl): 45 - 66.
Gunsolley JC, Zambon JJ, Mellott CA, Brooks CN, Kauqars CC. Periodontal theraphy in young adults with severe generalized periodontitis. J Periodontol. 1994; 65: 268 - 73.
Mombelli A, Schmid B, Rutar A, Lang NP. Persistence patterns of Porphyromonas gingivalis, Prevotella intermedia/nigrescens, and Actinobacillus actinomycetemcomitans after mechanical therapy of periodontal disease. J Periodontol. 2000; 71: 14 - 21.
Guerrero A, Griffiths GS, Nibali L, Suvan J, Moles DR, Laurell L, Tonetti MS. Adjunctive benefits of systemic amoxicillin and metronidazole in non-surgical treatment of generalized aggressive periodontitis: a randomized placebo-controlled clinical trial. J Clin Periodontol. 2005; 32: 1096 - 107.
Rabelo CC, Feres M, Goncalves C, Figueiredo C, Faveri M, Tu Y-K and Chambrone L. Systemic antibiotics in the treatment of aggressive periodontitis. A systematic review and a Bayesian Network meta-analysis. J Clinical Periodontol. 2015; 42: 647 - 57.
The Danish National Clinical Recommendations, 2016. Sundhedsstyrelsen, Islands Brygge 67, 2300 København S, Denmark. https: //www.sst.dk/da/udgivelser/2016/~/media/F5344E45B2FC48699B5C9F4D918DAB9B.ashx
Haffajee AD, Socransky SS, Gunsolley JC. Systematic anti-infective periodontal therapy. A systematic review. Ann Periodontol. 2003; 8: 115 - 81.
Winkel EG1, Van Winkelhoff AJ, Timmerman MF, Van der Velden U, Van der Weijden GA. Amoxicillin plus metronidazole in the treatment of adult periodontitis patients. A double-blind placebo-controlled study. J Clin Periodontol. 2001; 28: 296 - 305.
Keestra JAJ, Grosjean I, Coucke W, Quirynen M, Teughels W. Non-surgical periodontal therapy with the systemic antibiotics in patients with untreated chronic periodontitis: a systematic review and meta-analysis. J Periodont Res. 2015; 50: 294 - 314.
Cionca N, Giannopoulou C, Ugolotti G, Mombelli A. Amoxicillin and metronidazole as an adjunct to full-mouth scaling and root planing of chronic periodontitis. J Periodontol. 2009; 80: 364 - 71.
Cionca N, Giannopoulou C, Ugolotti G, Mombelli A. Microbiologic testing and outcomes of full-mouth scaling and root planing with or without amoxicillin/metronidazole in chronic periodontitis. J Periodontol. 2010; 81: 15 - 23.
van Winkelhoff AJ, Winkel EGAntibioics in Periodontics: Right or Wrong? J Periodontol. 2009; 80: 1555 - 8.
Preus HR, Gjermo P, Baelum V. A double-masked randomized clinical trial (RCT) comparing four periodontitis treatment strategies: 5-year clinical results. J Clinical Periodontol. 2017; 44: 1029 - 38.
Preus HR, Gjermo P, Baelum V. A randomized double-masked clinical trial comparing four periodontitis treatment strategies: 5-year tooth loss results. J Periodotol. 2017; 88: 144 - 52.
Lindhe J, Meyle J, Group DoEWoP. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008 Sep; 35 (8 Suppl): 282 - 5.
Serino G, Ström C. Peri-implantitis in partially edentulous patients: association with inadequate plaque control. Clin Oral Implants Res. 2009 Feb; 20(2): 169 - 74.
Jepsen S, Berglundh T, Genco R, Aass AM, Demirel K, Derks J, Figuero E, Giovannoli JL, Goldstein M, Lambert F, Ortiz-Vigon A, Polyzois I, Salvi GE, Schwarz F, Serino G, Tomasi C, Zitzmann NU. Primary prevention of peri-implantitis: managing peri-implant mucositis. J Clin Periodontol. 2015 Apr; 42 Suppl 16: S152 - 7.
Monje A, Aranda L, Diaz KT, Alarcón MA, Bagramian RA, Wang HL, Catena A. Impact of Maintenance Therapy for the Prevention of Peri-implant Diseases: A Systematic Review and Meta-analysis. J Dent Res. 2016 Apr; 95(4): 372 - 9.
Albrektsson T, Dahlin C, Jemt T, Sennerby L, Turri A, Wennerberg A. Is marginal bone loss around oral implants the result of a provoked foreign body reaction? Clin Implant Dent Relat Res. 2014 Apr; 16(2): 155 - 65.
Derks J, Tomasi C. Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol. 2015 Apr; 42 Suppl 16: S158 - 71.
Derks J, Schaller D, Håkansson J, Wennström JL, Tomasi C, Berglundh T. 2016 (a). Effectiveness of Implant Therapy Analyzed in a Swedish Population: Prevalence of Peri-implantitis. J Dent Res. J Dent Res. Jan; 95(1): 43 - 9.
Renvert S, Quirynen M. Risk indicators for peri-implantitis. A narrative review. Clin Oral Implants Res. 2015 Sep; 26 Suppl 11: 15 - 44.
Sgolastra F, Petrucci A, Severino M et al. Smoking and the risk of peri-implantitis. A systematic review and meta-analysis. Clin Oral Implants Res. 2015 Apr; 26(4): e62 - 7.
Dalago HR, Schuldt Filho G, Rodrigues MA et al. Risk indicators for peri-implantitis. A cross-sectional study with 916 implants. Clin Oral Implants Res. 2017 Feb; 28(2): 144 - 150.
Berglundh T, Zitzmann NU, Donati M. Are peri-implantitis lesions different from periodontitis lesions? J Clin Periodontol. 2011 Mar; 38 Suppl 11: 188 - 202.
Derks J, Schaller D, Håkansson J, Wennström JL, Tomasi C, Berglundh T. Peri-implantitis - onset and pattern of progression. J Clin Periodontol. 2016; Apr; 43(4): 383 - 8.
Charalampakis G, Leonhardt Å, Rabe P, Dahlén G. Clinical and microbiological characteristics of peri-implantitis cases: a retrospective multicentre study. Clin Oral Implants Res. 2012 Sep; 23(9): 1045 - 54.
Carcuac O, Derks J, Charalampakis, G, Abrahamsson I, Wennström J, Berglundh, T. Adjunctive systemic and local antimicrobial therapy in the surgical treatment of peri-implantitis: A randomized controlled clinical trial. J Dent Res. 2016 Jan; 95(1): 50 - 7.
Mombelli A, Marxer M, Gaberthüel T, Grunder U, Lang NP. The microbiota of osseointegrated implants in patients with a history of periodontal disease. J Clin Periodontol. 1995 Feb; 22(2): 124 - 30.
van Winkelhoff AJ, Goené RJ, Benschop C, Folmer T. Early colonization of dental implants by putative periodontal pathogens in partially edentulous patients. Clin Oral Implants Res. 2000 Dec; 11(6): 511 - 20.
Marsh P, Lewis MAO, Rogers H, Williams D, Wilson M. Marsh & Martin´s Oral Microbiology. Edinburgh: Elsevier; 2016.
Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL Jr. Microbial complexes in subgingival plaque. J Clin Periodontol. 1998 Feb; 25(2): 134 - 44.
Hajishengallis G, Darveau RP, Curtis MA. The keystone-pathogen hypothesis. Nat Rev Microbiol. 2012 Oct; 10(10): 717 - 25.
Hajishengallis G, Lamont RJ. Dancing with the Stars: How Choreographed Bacterial Interactions Dictate Nososymbiocity and Give Rise to Keystone Pathogens, Accessory Pathogens, and Pathobionts. Trends Microbiol. 2016 Jun; 24(6): 477 - 89.
Shiba T, Watanabe T, Kachi H, Koyanagi T, Maruyama N, Murase K, Takeuchi Y, Maruyama F, Izumi Y, Nakagawa I. Distinct interacting core taxa in co-occurrence networks enable discrimination of polymicrobial oral diseases with similar symptoms. Sci Rep. 2016 Aug 8; 6: 30997.
Kumar PS, Mason MR, Brooker MR, O'Brien K. Pyrosequencing reveals unique microbial signatures associated with healthy and failing dental implants. J Clin Periodontol. 2012 May; 39(5): 425 - 33.
Rakic M, Grusovin MG, Canullo L. The Microbiologic Profile Associated with Peri-Implantitis in Humans: A Systematic Review. Int J Oral Maxillofac Implants. 2016 Mar-Apr; 31(2): 359 - 68.
Lafaurie GI, Sabogal MA, Castillo DM, Rincon MV, Gomez LA, Lesmes YA, et al. Microbiome and Microbial Biofilm Profiles of Peri-Implantitis: A Systematic Review. J Periodontol. 2017 Oct; 88(10): 1066 - 89.
Zheng H, Xu L, Wang Z, Li L, Zhang J, Zhang Q, et al. Subgingival microbiome in patients with healthy and ailing dental implants. Sci Rep. 2015 Jun 16; 5: 10948.
Eick S, Ramseier CA, Rothenberger K, Brägger U, Buser D, Salvi GE. Microbiota at teeth and implants in partially edentulous patients. A 10-year retrospective study. Clin Oral Implants Res. 2016 Feb; 27(2): 218 - 25.
Persson GR, Renvert S. Cluster of bacteria associated with peri-implantitis. Clin Implant Dent Relat Res. 2014 Dec; 16(6): 783 - 93.
Belibasakis GN, Mir-Mari J, Sahrmann P, Sanz-Martin I, Schmidlin PR, Jung RE. Clinical association of Spirochaetes and Synergistetes with peri-implantitis. Clin Oral Implants Res. 2016 Jun; 27(6): 656 - 61.
Jankovic S, Aleksic Z, Dimitrijevic B, Lekovic V, Milinkovic I, Kenney B. Correlation between different genotypes of human cytomegalovirus and Epstein-Barr virus and peri-implant tissue status. Aust Dent J. 2011 Dec; 56(4): 382 - 8.
Slots J. Human viruses in periodontitis. Periodontol 2000. 2010 Jun; 53: 89 - 110.
Tsigarida AA, Dabdoub SM, Nagaraja HN, Kumar PS. The influence of smoking on the peri-implant microbiome. J Dent Res. 2015 Sep; 94(9): 1202 - 17.
Demmer RT, Jacobs DR Jr, Singh R, Zuk A, Rosenbaum M, Papapanou PN, Desvarieux M. Periodontal Bacteria and Prediabetes Prevalence in ORIGINS: The Oral Infections, Glucose Intolerance, and Insulin Resistance Study. J Dent Res. 2015 Sep; 94(9 Suppl): 201S-11S.
Ganesan SM, Joshi V, Fellows M, Dabdoub SM, Nagaraja HN, O'Donnell B, Deshpande NR, Kumar PS. A tale of two risks: smoking, diabetes and the subgingival microbiome. ISME J. 2017 Sep; 11(9): 2075 - 89.
Monje A, Catena A, Borgnakke WS. Association between diabetes mellitus/hyperglycaemia and peri-implant diseases: Systematic review and meta-analysis. J Clin Periodontol. 2017 Jun; 44(6): 636 - 48.
Edlund C, Hedberg M, Nord CE. Antimicrobial treatment of periodontal diseases disturbs the human ecology: a review. J Chemother. 1996 Oct; 8(5): 331 - 41.
O´Neill. 2014.Antimicrobial resistance: Tackling a crisis for the health and wealth of nations. https://amr-review.org/sites/default/files/AMR%20Review%20Paper%20-%20Tackling%20a%20crisis%20for%20the%20health%20and%20wealth%20of%20nations_1.pdf
World Health Organization. 2014. Antimicrobial resistance: Global report on surveillance. http://www.who.int/drugresistance/documents/surveillancereport/en/
Holmes AH, Moore LS, Sundsfjord A, Steinbakk M, Regmi S, Karkey A, Guerin PJ, Piddock LJ. Understanding the mechanisms and drivers of antimicrobial resistance. Lancet. 2016 Jan 9; 387(10014): 176 - 87.
Popa O, Dagan T. Trends and barriers to lateral gene transfer in prokaryotes. Curr Opin Microbiol. 2011 Oct; 14(5): 615 - 23.
Blair JM, Webber MA, Baylay AJ, Ogbolu DO, Piddock LJ. Molecular mechanisms of antibiotic resistance. Nat Rev Microbiol. 2015; 13(1): 42 - 51.
Cantón R, Ruiz-Garbajosa P. Co-resistance: an opportunity for the bacteria and resistance genes. Curr Opin Pharmacol. 2011 Oct; 11(5): 477 - 85.
Hyvarinen K, Laitinen S, Paju S, Hakala A, Suominen-Taipale L, Skurnik M, Kønønen E, Pussinen PJ. Detection and quantification of five major periodontal pathogens by single-copy gene-based real-time PCR. Innate Immun. 2009; 15: 195 - 204.
Loomer P. Microbiological testing in the treatment of periodontal diseases. Periodontol 2000. 2004; 34: 49 - 56.
Socransky SS, Smith C, Martin L, Paster BJ, Dewhirst FE, Levin AE. «Checkerboard» DNA-DNA hybridization. Biotechniques. 1994Oct; 17(4): 788 - 92.
Livermore DM. Minimising antibiotic resistance. Lancet Infect Dis. 2005 Jul; 5(7): 450 - 9.
Foucault C, and Brouqui P. How to fight antimicrobial resistance. FEMS Immunol Med Microbiol. 2007 Mar; 49 (2): 173 - 83.
Jönsson M, Swedberg G. Macrolide resistance can be transferred by conjugation from viridans streptococci to Streptococcus pyogenes. Int J Antimicrob Agents. 2006 Aug; 28(2): 101 - 3.
Rams TE, Degener JE, van Winkelhoff AJ. Antibiotic resistance in human peri-implantitis microbiota. Clin Oral Implants Res. 2014 Jan; 25(1): 82 - 90.
Olsen I, Solberg CO, Finegold SM. A primer on anaerobic bacteria and anaerobic infections for the uninitiated. Infection. 1999 May-Jun; 27 (3): 159 - 65.
Verdugo F, Laksmana T, Uribarri A. Systemic antibiotics and the risk of superinfection in peri-implantitis. Arch Oral Biol. 2016 Apr; 64: 39 - 50.
Gomi K, Matsushima Y, Ujiie Y, Shirakawa S, Nagano T, Kanazashi M, Yashima A. Full-mouth scaling and root planing combined with azithromycin to treat peri-implantitis. Aust Dent J. 2015 Dec; 60(4): 503 - 10.
Heitz-Mayfield LJ, Salvi GE, Mombelli A, Faddy M, Lang NP. Implant Complication Research Group. Anti-infective surgical therapy of peri-implantitis. A 12-month prospective clinical study. Clin Oral Implants Res. 2012. Feb; 23(2): 205 - 10.
Bush K, Bradford PA. ?-Lactams and ?-Lactamase Inhibitors: An Overview. Cold Spring Harb Perspect Med. 2016 Aug 1; 6 (8).
Georgopapadakou NH, Liu FY. Penicillin-binding proteins in bacteria. Antimicrob Agents Chemother. 1980 Jul; 18(1): 148 - 57.
Pagès JM, James CE, Winterhalter M. The porin and the permeating antibiotic: a selective diffusion barrier in Gram-negative bacteria. Nat Rev Microbiol. 2008 Dec; 6(12): 893 - 903.
Tang SS, Apisarnthanarak A, Hsu LY. Mechanisms of ?-lactam antimicrobial resistance and epidemiology of major community- and healthcare-associated multidrug-resistant bacteria. Adv Drug Deliv Rev. 2014 Nov 30; 78: 3 - 13.
Hackbarth CJ, Chambers HF. Methicillin-resistant staphylococci: genetics and mechanisms of resistance. Antimicrob Agents Chemother. 1989 Jul; 33(7): 991 - 4.
Hakenbeck R, Coyette J. Resistant penicillin-binding proteins. Cell Mol Life Sci. 1998 Apr; 54(4): 332 - 40.
Horn R, Lavallée J, Robson HG. Susceptibilities of members of the Bacteroides fragilis group to 11 antimicrobial agents. Antimicrob Agents Chemother. 1992 Sep; 36(9): 2051 - 3.
Bradford PA. Extended-spectrum beta-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clin Microbiol Rev. 2001 Oct; 14(4): 933 - 51.
D'Angelo RG, Johnson JK, Bork JT, Heil EL. Treatment options for extended-spectrum beta-lactamase (ESBL) and AmpC-producing bacteria. Expert Opin Pharmacother. 2016; 17(7): 953 - 67.
Poirel L, Kieffer N, Liassine N, Thanh D, Nordmann P. Plasmid-mediated carbapenem and colistin resistance in a clinical isolate of Escherichia coli. Lancet Infect Dis. 2016 Mar; 16(3): 281.
World Health Organization, 2017. Prioritization of pathogens to guide discovery, research and development of new antibiotics for drug-resistant bacterial infections, including tuberculosis. Geneva: World Health Organization; 2017(WHO/EMP/IAU/2017.12).
Schwarz S, Shen J, Kadlec K, Wang Y, Brenner Michael G, Feßler AT, Vester B. Lincosamides, Streptogramins, Phenicols, and Pleuromutilins: Mode of Action and Mechanisms of Resistance. Cold Spring Harb Perspect Med. 2016 Nov 1; 6(11).
Spízek J, Novotná J, Rezanka T. Lincosamides: chemical structure, biosynthesis, mechanism of action, resistance, and applications. Adv Appl Microbiol. 2004; 56: 121 - 54.
Boyanova L, Kolarov R, Mitov I. Recent evolution of antibiotic resistance in anaerobes as compared to previous decades. Anaerobe. 2015 Feb; 31: 4 - 10.
Hansen KCM, Schwensen SAF, Henriksen DP, Justesen US, Sydenham TV. Antimicrobial resistance in Bacteriodes fragilis group in faecal samples from patients receiving broad-spectrum antibiotics. Anaerobe. 2017; 47: 79 - 85.
Brook I. Spectrum and treatment of anaerobic infections. Journal of Infection and Chemotherapy. 2016; 22: 1 - 13.
Dingsdag SA, Hunter N. Metronidazole: an update on metabolism, structure-cytotoxicity and resistance mechanisms. J Antimicrob Chemother. 2018 Feb 1; 73(2): 265 - 79.
Drlica K, Hiasa H, Kerns R, Malik M, Mustaev A, Zhao X. Quinolones: Action and resistance updated. Curr Top Med Chem. 2009; 9 (11): 981 - 98.
Aldred KJ, Kerns RJ, Osheroff N. Mechanism of quinolone action and resistance. Biochemistry. 2014 Mar 18; 53(10): 1565 - 74.
Hawkey PM. Mechanisms of quinolone action and microbial response. J Antimicrob Chemother. 2003 May; 51 Suppl 1: 29 - 35.
Brodersen DE, Clemons WM Jr, Carter AP, Morgan-Warren RJ, Wimberly BT, Ramakrishnan V. The structural basis for the action of the antibiotics tetracycline, pactamycin, and hygromycin B on the 30S ribosomal subunit. Cell. 2000 Dec 22; 103(7): 1143 - 54.
Pioletti M, Schlünzen F, Harms J, Zarivach R, Glühmann M, Avila H, Bashan A, Bartels H, Auerbach T, Jacobi C, Hartsch T, Yonath A, Franceschi F. Crystal structures of complexes of the small ribosomal subunit with tetracycline, edeine and IF3. EMBO J. 2001 Apr 17; 20(8): 1829 - 39.
Grossman TH. Tetracycline Antibiotics and Resistance. Cold Spring Harb Perspect Med. 2016 Apr 1; 6(4): a025387.
Kannan K, Kanabar P, Schryer D, Florin T, Oh E, Bahroos N, Tenson T, Weissman JS, Mankin AS. The general mode of translation inhibition by macrolide antibiotics. Proc Natl Acad Sci U S A. 2014 Nov 11; 111(45): 15958 - 63.
Fyfe C, Grossman TH, Kerstein K, Sutcliffe J. Resistance to Macrolide Antibiotics in Public Health Pathogens. Cold Spring Harb Perspect Med. 2016 Oct 3; 6(10).
Weisblum B. Erythromycin resistance by ribosome modification. Antimicrob Agents Chemother. 1995; 39: 577 - 85.
Roberts MC. Update on macrolide-lincosamide-streptogramin, ketolide, and oxazolidinone resistance genes. FEMS Microbiol Lett. 2008; 282: 147 - 59.
Wolter N, Smith AM, Low DE, Klugman KPHigh-level telithromycin resistance in a clinical isolate of Streptococcus pneumoniae. Antimicrob Agents Chemother. 2007; 51: 1092 - 95.
Faccone D, Andres P, Galas M, Tokumoto M, Rosato A, Corso A. Emergence of a Streptococcus pneumoniae clinical isolate highly resistant to telithromycin and fluoroquinolones. J Clin Microbiol. 2005 43: 5800 - 5803.
Poehlsgaard J, Douthwaite S. The bacterial ribosome as a target for antibiotics. Nat Rev Microbiol. 2005 Nov; 3(11): 870 - 81.
Morar M, Pengelly K, Koteva K, Wright GD. Mechanism and diversity of the erythromycin esterase family of enzymes. Biochemistry. 2012; 51: 1740 - 51.
Chesneau O, Tsvetkova K, Courvalin P. Resistance phenotypes conferred by macrolide phosphotransferases. FEMS Microbiol Lett. 2007 Apr; 269 (2): 317 - 22.
Pavici? MJ, van Winkelhoff AJ, de Graaff J. Synergistic effects between amoxicillin, metronidazole, and the hydroxymetabolite of metronidazole against Actinobacillus actinomycetemcomitans. Antimicrob Agents Chemother. 1991; 35: 961 - 6.
Walker BC, Karpina K. Rational for use of antibiotics in periodontitis. J Periodontol. 2002; 73: 1188 - 96.
Kirkwood KL, Cirelli JA, Rogers JE, Giannobile WV. Novel host response therapeutic approaches to treat periodontal diseases. Periodontol 2000. 2007; 43: 294 - 315.
Renvert S, Polyzois I. Treatment of pathologic peri-implant pockets. Periodontol 2000. 2018 Feb; 76(1): 180 - 90.
Mombelli A, Lang NP. The diagnosis and treatment of peri-implantitis. Periodontol 2000. 1998 Jun; 17: 63 - 76.
Serino G, Turri A. Outcome of surgical treatment of peri-implantitis: results from a 2-year prospective clinical study in humans. Clin Oral Implants Res. 2011 Nov; 22(11): 1214 - 20.
Heitz-Mayfield LJA, Salvi GE, Mombelli A, Loup PJ, Heitz F, Kruger E, Lang NP. Supportive peri-implant therapy following anti-infective surgical peri-implantitis treatment: 5-year survival and success. Clin Oral Implants Res. 2018 Jan; 29(1): 1 - 6.
Carcuac O, Derks J, Abrahamsson I, Wennström JL, Petzold M, Berglundh T. Surgical treatment of peri-implantitis: 3-year results from a randomized controlled clinical trial. J Clin Periodontol. 2017 Dec; 44(12): 1294 - 303.
Hirsch R, Deng H, Laohachai MN. Azithromycin in periodontal treatment: more than an antibiotic. J Periodontal Res. 2012; 47(2): 137 - 48.
Hallström H, Persson GR, Lindgren S, Renvert S. Open flap debridement of peri-implantitis with or without adjunctive systemic antibiotics: A randomized clinical trial. J Clin Periodontol. 2017.Dec; 44(12): 1285 - 1293.
Corresponding author: Morten Enersen, Institute of Oral Biology, Faculty of Dentistry, University of Oslo, P.O. Box 1052, NO-0316 Oslo, Norway. E-mail: morteene@odont.uio.noArtikkelen har gjennomgått ekstern faglig vurdering.Enersen M, Hultin M, Kønønen E, Poulsen AH, Simm R. Antibiotics in the treatment of periodontal and peri-implant infections. Nor Tannlegeforen Tid. 2019; 129: 224 - 35
Institute of Oral Biology, Faculty of Dentistry University of Oslo, Oslo Norway
Department of Dental Medicine, Division of Periodontology, Karolinska Institutet, Huddinge, Sweden
Institute of Dentistry, Department of Periodontology, University of Turku, Turku, Finland
Department of Odontology, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark
Institute of Oral Biology, Faculty of Dentistry University of Oslo, Oslo Norway