Anca Virtej, Emma Wigsten, Dag Ørstavik, Sivakami Rethnam Haug
Future Directions in Endodontics
Associate Professor, DDS, PhD, Department of Clinical Dentistry, Faculty of Medicine, University of Bergen and Postdoc at Department of Oral Surgery, Haukeland University Hospital, Bergen, Norway.
DDS, PhD, Department of Endodontology, Institute of Odontology, The Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden.
Professor Emeritus, Dr. Odont., Department of Clinical Dentistry, Faculty of Dentistry, University of Oslo, Oslo, Norway.
Associate Professor, DDS, Dr. Odont, Department of Clinical Dentistry, Faculty of Medicine, University of Bergen, Bergen, Norway.
Headlines
Dental practitioners should have better communication with the patients about treatment goals and prognosis or refer to a specialist at the appropriate time without delays to achieve optimal treatment outcome.
Research must not only concentrate on innovations which may interest stakeholders with short-term benefits but on randomized studies, to compare with existing materials, to prove their superiority in clinical outcomes.
We need better knowledge to understand dental pain mechanisms, management of pain sensation, control and eradicate infection.
Recruitment of students with outstanding performances by educational institutions in a competitive job market is a challenge that needs to be addressed.
The cost of dental treatment, including endodontics, may call for increased third-party payment by government or private insurance schemes. By studying the cost-effectiveness of treatment, current systems may need to be reviewed.
Preserving a tooth with root canal treatment (RCT) has a positive impact on the patient’s oral health-related quality of life. However, cross-sectional studies show that technical quality of root fillings is less than optimal. In the future, more dental practitioners need to evaluate case difficulty and decide on whether they want to treat a tooth or refer to a specialist. The concept of minimally invasive treatment has been advocated during cavity preparation, instrumentation, and regenerative procedures. Unfortunately, long-term clinical outcome studies are lacking in this area. Research in pain mechanisms, inflammatory processes, the impact of systemic health on disease progression, and healing mechanisms is scarce. Infection control, antibiotic resistance and new antibacterial treatment regiments are issues to address in the future. We may anticipate increased regulation and administration of dental, including endodontic, services through insurance schemes and government involvement. Improved quality of service provision through a high standard of dental education is the most important investment to shape endodontics in the future. Health authorities and media may then present endodontic treatment as a safe, reliable, and effective option that is performed to benefit patients.
Figure 1. The future direction is something we believe will happen or something we want to happen.
“Declare the past, diagnose the present, foretell the future” – Hippocrates, ca. 460 BC.
“Future” refers to that will happen or exist after the present time. A “direction” is the general way in which something develops or progresses (Fig. 1). In this article, we present the current status in endodontic treatment, recent developments and the authors’ opinions on in which direction the endodontic discipline ought to develop in the future. This article has organized future directions into three parts, namely, the patient, the dental practitioner, and national or societal level.
The patient
In recent decades, oral health has generally improved in the Nordic countries. At the same time, life expectancy has increased, which means that more and more people retain their natural dentition into old age and fewer become edentulous. More teeth therefore risk having a history of dental treatment causing injury to the dental pulp with subsequent pulp disease [1]. Root canal treatment (RCT) is mostly undertaken in general dental practice. In the Swedish Social Insurance Agency’s (SSIA’s) data register, 217,047 residents above 20 years of age were registered as receiving RCT on at least one tooth in 2009 [2]. Ten years later, almost 190,000 teeth were registered as root filled in the same data register, pointing at a decrease in endodontic treatments [3]. A similar trend was also observed in Denmark (Danish Civil Registration System) during the period 1997-2009. In addition, Razdan et al. (2022) [4] observed that while the number of root filled teeth decreased, the incidence of apical periodontitis in non-root filled teeth increased. National registries on dental treatment combined with epidemiological studies have the potential to detect trends in endodontic treatment needs in a population, which is helpful to identify changes relevant to education and insurance systems, and thereby promote dental health.
Preserving a tooth with RCT has a positive impact on the patient’s oral health-related quality of life. Endodontic treatment ought to be promoted as a safe, reliable and effective alternative that patients can benefit from and for this, the health authorities and media are of great importance. Patients are generally satisfied with their endodontic treatment and prefer to keep their natural dentition whenever possible [5][6][7][8]. When treatment was evaluated by studying the patient’s experience more specifically, through so-called patient satisfaction [7], patients who underwent treatment, both in specialist and general dental care were satisfied with their choice and their treatment [7][9]. The factor showing the least degree of satisfaction was the cost. It is important to involve the patient in their treatment plan and process, along with identifying common goals for the clinical outcome (Fig. 2). The success or failure of the treatment should be determined on the basis of predefined goal(s) for each individual [6], where communication plays a key role. Patients need to be aware that seeking treatment at the appropriate time (without delays) is vital to achieve optimal treatment outcome.
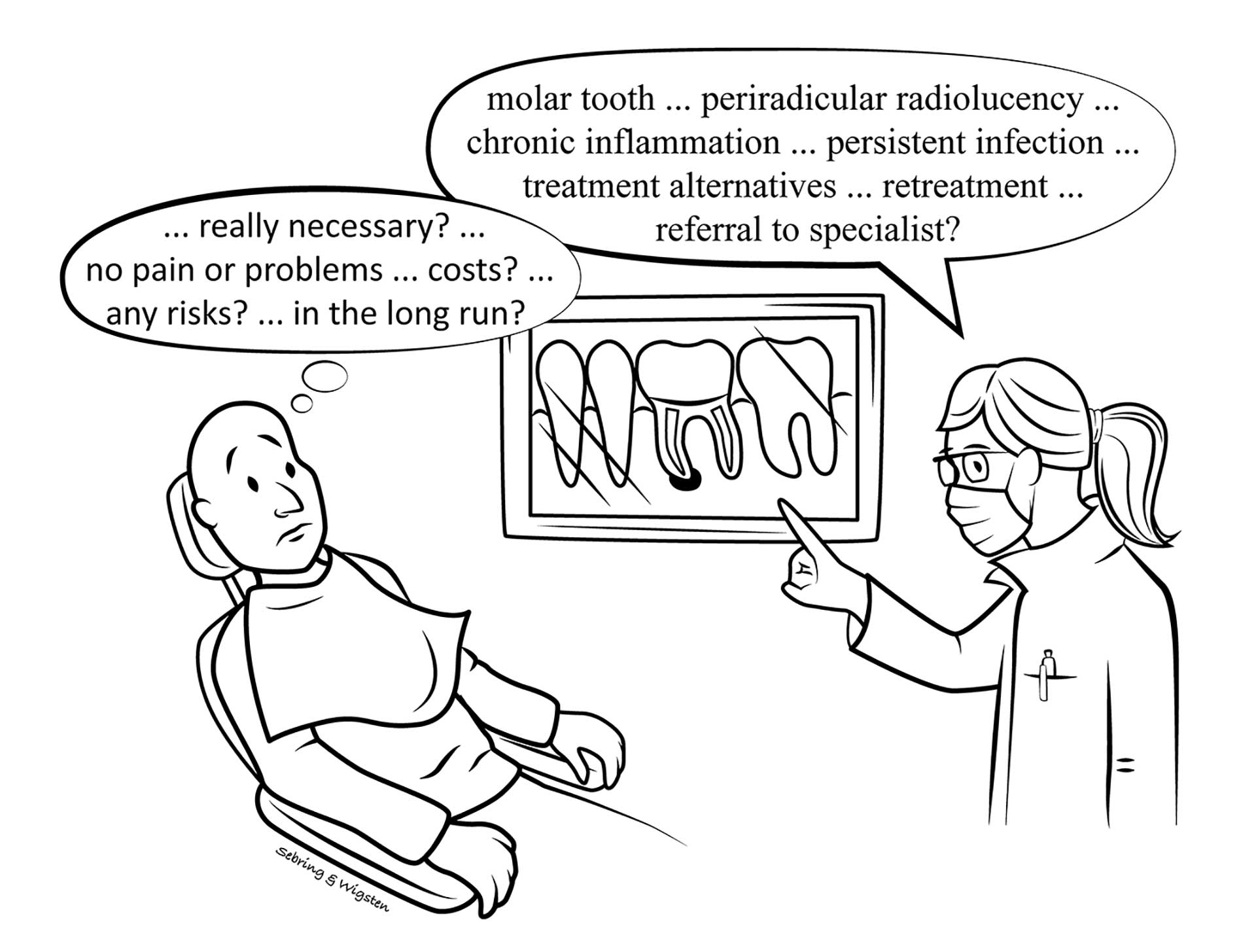
Figure 2. The goal of RCT is to preserve the affected tooth and establish or maintain healthy peri-radicular tissues. However, the individual patient, who is generally unaware of the status of the tooth, does not necessarily share the same concerns. It may also be the case that the patient and the dentist have different views on what is considered important and what characterizes a successful treatment [5][6].
Dental Practitioners
RCT can be perceived as technically demanding, stressful and frustrating, and associated with loss of control [10]. Almost half of the cases that were referred to a specialist clinic in Västra Götaland, Sweden, were previously root filled molars needing additional endodontic treatment [11]. RCT of molar teeth in general dental practice are often reported to have a poorer technical quality of the root filling, higher incidence of periapical disease, and lower survival rate compared to other tooth groups [12][13]. There can be many reasons for this: molar teeth usually have more roots, a more complex root canal anatomy and a placement in the dental arch which is difficult to access. Molars are not only technically demanding, but also often associated with complications during treatment thereby requiring more resources [14]. However, an anterior tooth or a premolar can also pose difficulties when the pulp chamber and root canal system is reduced in dimension, or when the root is severely curved [15]. The lower success rate, coupled with the experience of stress and frustration concerning treatment, raises the question as to who should perform the endodontic treatment, the general practitioner, or the specialist [10]?
A good understanding of case difficulty and operator abilities can help general practitioners decide on whether they should treat a tooth or refer to a specialist for the benefit of the patient.
Endodontic diagnosis
The major cause of endodontic disease is infection by microorganisms. New techniques for detection of bacteria in the root canal offer some hope that chairside determination of infecting microorganisms may be possible in the future [16]. Recent research has also focused on the identification of biomarkers to establish the inflammatory state of the dental pulp or periapical tissues (Fig. 3). Host molecules, both systemic and local, can theoretically be measured and linked to endodontic disease or treatment outcome [17][18]. We may hope that, in the not too distant future, user-friendly and accurate chairside methods for pulpal and periapical diagnosis may become generally available [19]. However, extensive, and time-consuming translational research will be necessary to apply new knowledge from sterile laboratory studies to the development of reliable clinical methods for chair-side patient diagnosis.
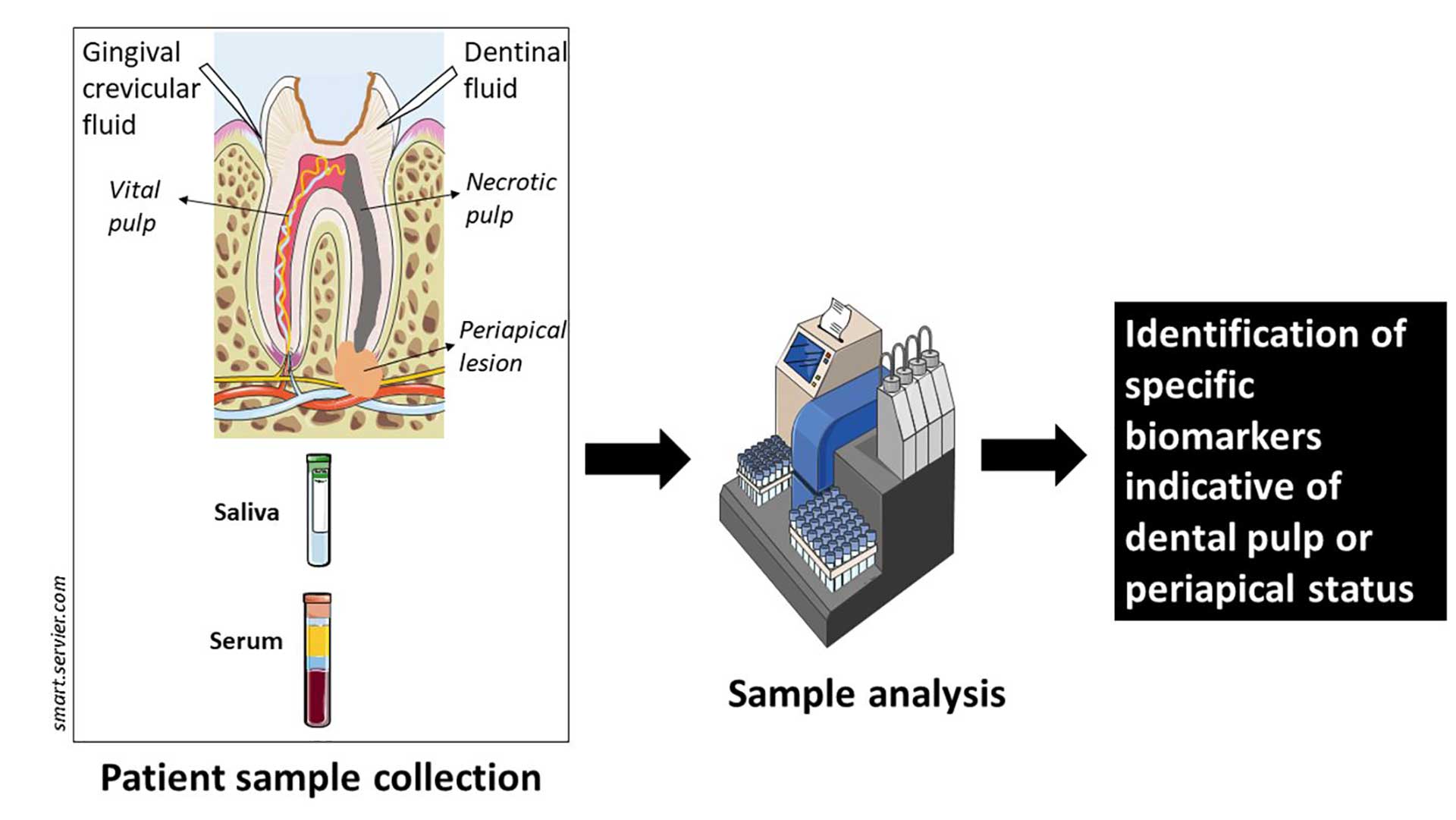
Figure 3. Samples from serum, saliva, gingival crevicular or dentinal fluid are collected, analyzed at molecular level to establish diagnosis and optimal treatment.
Cone-beam computer tomography (CBCT) is a three-dimensional radiographic technique which overcomes the anatomical noise and diagnostic limitations of two-dimensional periapical radiographs (Fig. 4). The European Society of Endodontology (ESE) advises the inclusion of CBCT-related education in the curricula of dental under-and postgraduate education [20]. There is an increase in acquisition of CBCT scanners by dental specialist clinics in USA and Scandinavia; however, implant treatment planning has so far been the major indication for CBCT scans in Norway and Sweden [21][22]. Considerations need to be made regarding risks and benefits of exposing the patient to ionizing radiation, but technology is improving. Future CBCT scanners with reduced radiation dosage are expected to be commonplace in dental practice and aid in endodontic diagnoses and treatment planning.

Figure 4. The apical diagnosis of teeth 15-17 was uncertain following a periapical radiograph and fistulography (A). A CBCT scan confirms periapical lesions extending from second premolar to second molar (B and C).
Artificial intelligence (AI) is a branch of applied computer science originating in the 1950s and refers to the idea of building machines that will be able to perform tasks normally carried out by humans [23]. AI and machine learning systems have the potential to revolutionize dentistry by improving reliability and reach accurate diagnosis [23]. AI can potentially aid in detecting periapical lesions, vertical root fractures, working length determination or predicting endodontic treatment outcomes in the future. Reliability and applicability of AI need to be verified before use in day-to-day clinical practice [24].
Access cavity preparation
The medical field is in an age of minimally invasive treatments. Minimally invasive access cavity preparation or a “ninja-approach” to the root canal system has been advocated to preserve dentine and minimize risk of tooth fracture [25]. The technique moves away from the traditional straight-line access. While preserving coronal tooth substance, parts of the pulp chamber roof that may be infected are left in place during the entire treatment course. Furthermore,, this approach increases the difficulty of subsequent treatment steps, such as root canal localization and instrumentation, and undermines infection control [26]. Another new technique is guided access cavity preparation. Briefly, this technique involves preoperative CBCT scans, fabrication of templates for guidance of specialized burs to locate canals with minimal preparation and finally instrumentation [27]. However, it is questionable if we should subject all patients to a CBCT scan without evidence-based benefit for dentine preservation. Furthermore, there are, currently no long-term clinical outcome studies on minimally invasive or guided access cavity preparations to indicate that they are superior or even similar to the current access cavity preparation principles and methods.
Infection control
Aseptic techniques are of paramount importance during endodontic procedures. Correct hand hygiene, rubber dam use and disinfection of the endodontic operative field are essential steps in an aseptic endodontic treatment course [28]. Rubber dam was introduced to the dental profession in 1864 and is the standard of care for all endodontic procedures (Fig. 5). Despite this,, usage of rubber dam varies greatly between countries. In Denmark, most dentists do not consistently use rubber dam [29]. In Finland, only about 30% of endodontic treatments are performed under rubber dam [30]. Ultimately, we need to be reminded that the results of all endodontic treatments are infection related [31][32). No other effective isolation techniques are available for now and the professional and legal pressure to use rubber dam during endodontic procedures should be strengthened in the future.
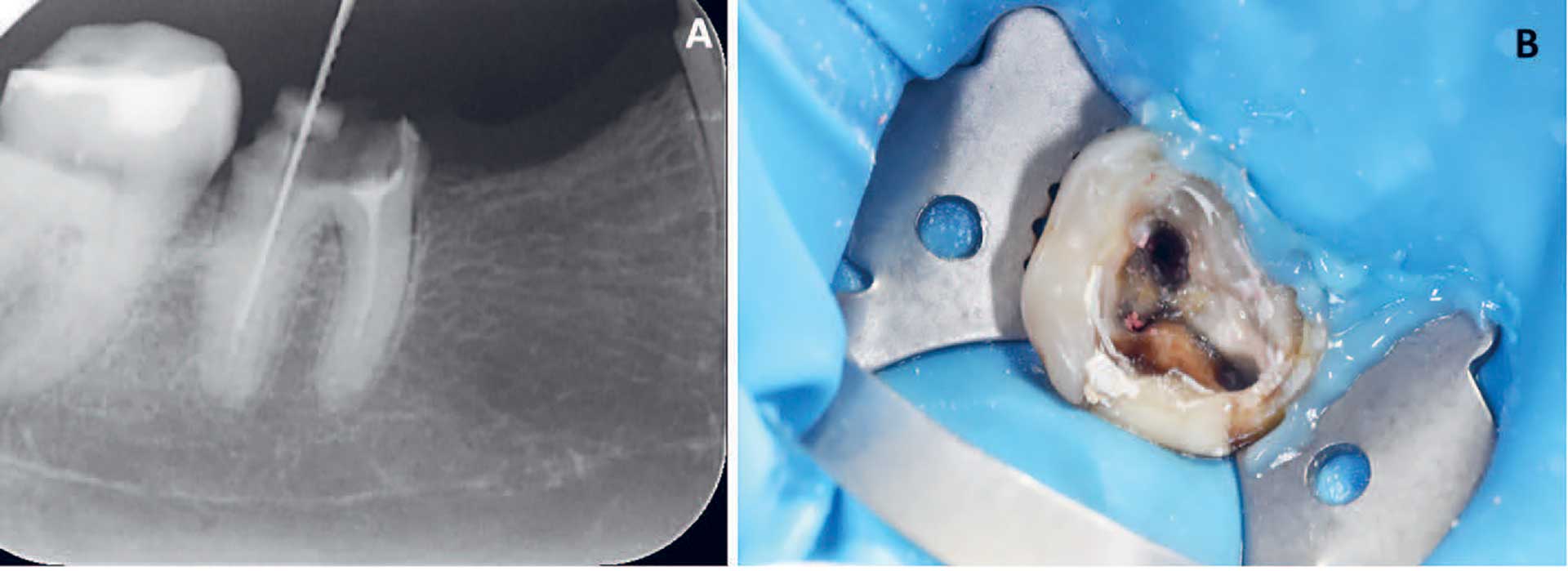
Figure 5. In Norway and Sweden, more dentists routinely use rubber dam during endodontic procedures [31], with a higher frequency among younger dentists (64). Yet only very few Norwegian dentists seal the area between rubber dam and tooth in comparison to an overwhelming majority of Swedish GDPs [31]. Here exemplified is (A) a working length radiograph taken without rubber dam which endangers the patient and can impair treatment course; (B) correct placement of rubber dam on a molar tooth increases visibility and access, along with providing better infection control.
Root canal infection is still the most common cause for treatment failure [32]. New instrumentation and irrigation techniques and protocols are continuously being developed to improve canal disinfection. Disinfectants such as 2% chlorhexidine have not shown superiority to sodium hypochlorite (NaOCl) use during chemomechanical preparations [33]. Multisonic irrigant activation may increase root canal cleanliness [34][35]. The use of engine-driven Ni-Ti single file systems for instrumentation has become commonplace in the last decade. Single-file techniques are associated with shortened preparation time, and single-visit approaches to treatment also reduces the time for disinfection. To achieve antibacterial effectiveness, NaOCl in low concentrations requires large volumes and frequent applications [36]. Thus, while reduced treatment time has economical and practical advantages, it may have a negative impact on the time spent on irrigation and associated antibacterial effect and may not effectively reduce microorganisms in the root canal system.
Intracanal medications have unfortunately undergone minimal innovation. Calcium hydroxide, a substance introduced in 1920, is still the first choice of intracanal medicament. Bacteria establish colonies not just in the main root canals, but also in dentinal tubuli, lateral and accessory canals, isthmuses, and anastomoses, which are locations that cannot be reliably reached by instrumentation and irrigation alone [37]. Microorganisms such as E. faecalis or C. albicans are often encountered in secondary infections and are known to resist the effects of calcium hydroxide [38][39]. While not available to clinical use yet, the antimicrobial and immunomodulating activity of probiotics applied in the root canal may target endodontic pathogens in the future [40].
Odontogenic infections of endodontic origin may require antibiotic treatments when they affect systemic health. Yet, antibiotic use in the dental practice is often empirical and can be inappropriate, as a bacteriological sensitivity test is rarely performed [41]. Antibiotic sensitivity of bacteria is decreasing globally [42][43], and this also affects strains residing in the oral cavity [44], in particular Porphyromonas spp. and Prevotella spp. [45]. There is a possibility that microorganisms causing endodontic infections may become resistant to antibiotics in the future. Rapid point-of-care diagnostic tests providing information on the pathogen and its susceptibility to antibiotics may have great potential to minimise inappropriate antibiotic use and to increase patients’ safety [42].
Root filling materials
Filling the root canal system is the final step of endodontic treatment and aims at closing the door to bacteria and to oral and periapical fluids. The most common core material in root fillings is still gutta-percha, but new sealers are being constantly introduced. Yet, shortcomings of sealers, such as shrinkage, solubility, or lack of bonding to the gutta-percha core, may influence treatment outcome [46]. A promising choice in the future comes from bioceramic sealers due to their antibacterial properties, dimensional stability and their bioreactivity. New endodontic materials and techniques are often marketed by ‘pretty’ periapical radiographs advertised on social media by manufacturers and experts with lack of clinical data on outcome [26][47]. As such, our material choices should ideally be backed by clinically relevant research on biomaterials.
Regeneration in endodontics
Regenerative treatment of necrotic teeth with open apex which allows further growth of dental tissues have long been in clinical practice. The procedure relies on stem cells from the apical papilla that can enter the root canal space, differentiate, and continue root development [48]. Theoretically, dental pulp stem cells (DPSC) can also differentiate and regenerate pulp tissue contributing to minimally invasive treatment of mature teeth. Progression from stem cells into differentiated cells requires epigenetic modifications, as exemplified and detailed in Figure 6. Yet, availability of autologous DPSC is limited [49]. The American Association of Endodontists (AAE) and ESE have not yet recommended autologous DPSC transplantation in clinical regenerative endodontics, because of complex and expensive technical requirements, government regulatory issues, and not least clinician’s training and skills [50]. In the future, these barriers may be overcome and it may be possible to treat inflamed and necrotic dental pulps by regeneration via tissue engineering [51].
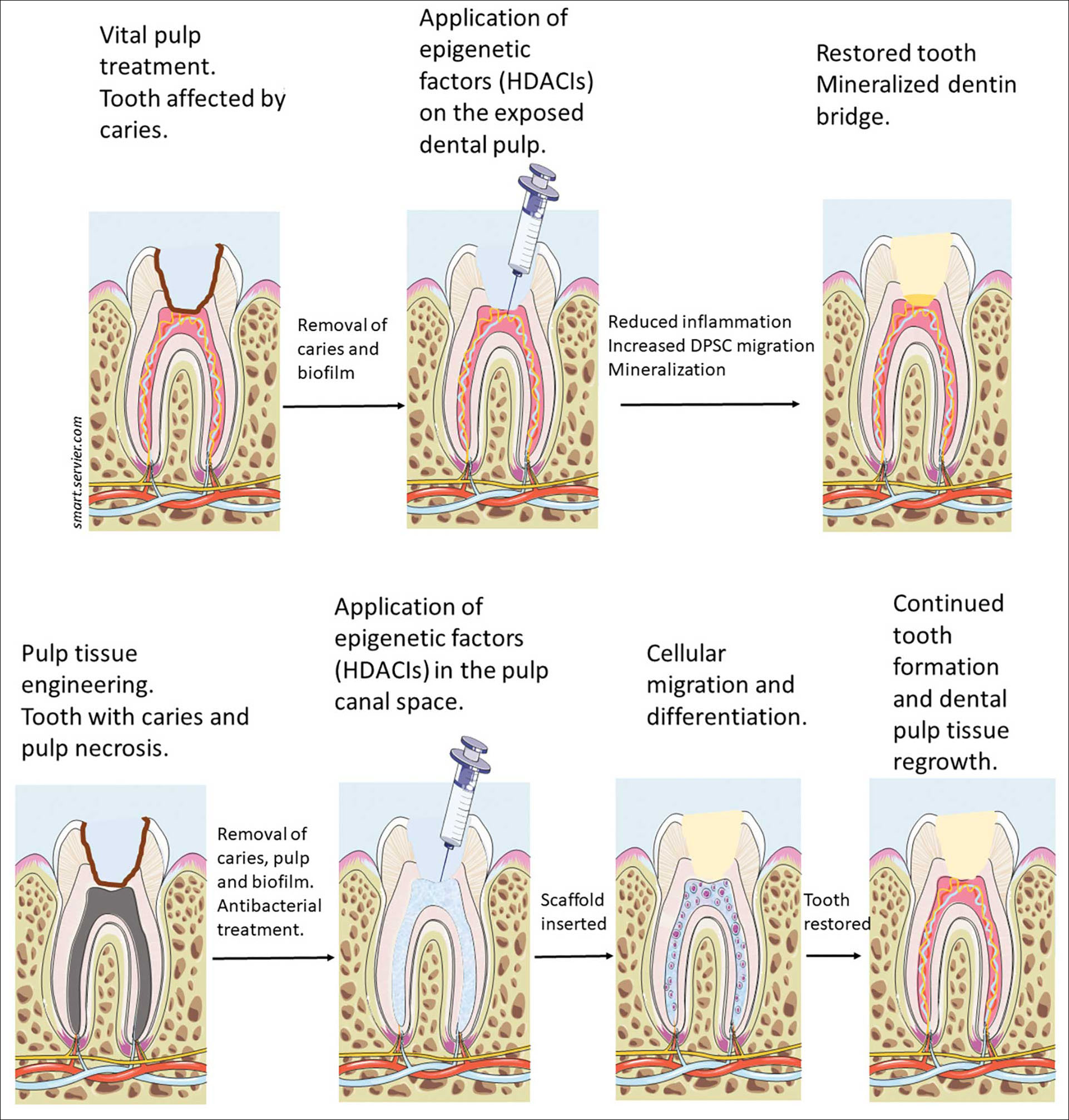
Figure 6. Example for epigenetic modifications that can be used as treatment of the vital and necrotic dental pulp, modified after [51]. DNA consists of histones. Acetylation and deacetylation of histones play an important role in transcription regulation of cells. Histone deacetylases (HDAC) are linked to human disease, while their inhibitors, HDACis are a promising aid in treating several illnesses, including inflammation [65][66]. Once the caries and biofilm are removed, HDACis are topically applied to an exposed dental pulp to reduce inflammation, increase dentin mineralization and DPSC migration, along with formation of new blood vessels, restoring the integrity of the tooth (upper panel). Revitalization procedures, meaning continued root formation and regrowth of vital tissue in the pulp canal space are also the aim of this technology in the future, as seen in the lower panel.
The national or societal level
Dental Education
Dental education is the most important investment to shape the future of endodontics. Students today will be our future dental educators, policy makers, specialists, researchers, as well as general practitioners. Training during undergraduate education is integral to build confidence and security [52]. A recent survey showed that more than 70% of general dentists felt that they did not receive adequate clinical training [53]. Requirements for endodontic treatment in dental schools vary and the number of cases suitable for student treatment are somewhat limited in some institutions [52][54][55]. This may result in newly qualified students who appear to lack recommended competencies [56]. Lifelong learning or continuing dental education is an integral part of dental education but cannot replace an inadequate undergraduate education [57][58]. Therefore, strengthening and supporting dental educators in teaching institutions needs to be highlighted. Recruitment of students with outstanding performances by educational institutions in a competitive job market is a challenge that needs to be addressed.
Research
At the end of the 20th century innovations such as the dental operating microscope, engine-driven instrumentation and apex locators were introduced to clinical endodontics. These technological advances in endodontics have made it possible for us to retain teeth that would have been extracted a few decades ago. Furthermore, advances in endodontic microsurgery have greatly increased treatment outcome [59].
Unfortunately, there is a lack of sources for research funding in dentistry [60]. Innovations are driven by stakeholders such as dental industry. Pain is still the reason why most patients seek dental treatment and RCT is still considered a painful procedure among the public [61][62]. Our understanding of pain mechanisms, inflammatory process, the impact of systemic health on disease progression, and healing mechanisms is limited [63]. Furthermore, infection control, dealing with antibiotic resistant bacteria, and new treatment regimens are lacking. Future research must not only concentrate on technical advances but also on topics such as basic science which may not interest stakeholders with short-term interests.
Cost and health authorities
While cost is a factor operating on all levels, systematic cost reduction can only be achieved through the involvement of insurance, either private or governmental. The Nordic dental care is financed for the most part by the adult paying population. Cost for endodontic treatment should ideally be compared with cost of replacement therapy by prosthodontic therapies [8]. It is also costly to educate and train specialists to provide endodontic treatment. Additional insurance may be needed to cover expenses for endodontic treatments should patients want to retain healthy natural teeth throughout their lifetime. In the future, we need regulation and administration of dental, including endodontic, services through insurance schemes and government involvement.
Conclusions
In the future technical advances to optimize endodontic treatment and prognosis need to be supplemented with better diagnostic methods, improved understanding of the disease process including mechanisms of for example pain and inflammation. For this, high-quality research on basic, translational, and clinical levels is necessary. In addition, well-financed insurance systems promoting dental health and including national documentation of treatments can enable research and identification of trends on societal level. Last, but not least, evidence-based and up-to date dental education may be the most important investment for the future.
References
Bjørndal L, Reit C. The annual frequency of root fillings, tooth extractions and pulp-related procedures in Danish adults during 1977-2003. Int Endod J. 2004;37(11):782-8.
Fransson H, Dawson VS, Frisk F, Bjørndal L, EndoReCo, Kvist T. Survival of Root-filled Teeth in the Swedish Adult Population. J Endod. 2016;42(2):216-20.
Försäkringskassan. Statistik inom tandvårdsområdet [Internet]. Stockholm: Försäkringskassan; 2021 [updated cited 2021-04-08]. Available from forsakringskassan.se, (opened 27.06.2022).
Razdan A, Jungnickel L, Schropp L, Vaeth M, Kirkevang LL. Trends of endodontic and periapical status in adult Danish populations from 1997 to 2009: A repeated cross-sectional study. Int Endod J. 2022;55(2):164-76.
Azarpazhooh A, Dao T, Ungar WJ, Da Costa J, Figueiredo R, Krahn M, et al. Patients’ Values Related to Treatment Options for Teeth with Apical Periodontitis. J Endod. 2016;42(3):365-70.
Friedman S, Mor C. The success of endodontic therapy--healing and functionality. J Calif Dent Assoc. 2004;32(6):493-503.
Dugas NN, Lawrence HP, Teplitsky P, Friedman S. Quality of life and satisfaction outcomes of endodontic treatment. J Endod. 2002;28(12):819-27.
Gatten DL, Riedy CA, Hong SK, Johnson JD, Cohenca N. Quality of life of endodontically treated versus implant treated patients: a University-based qualitative research study. J Endod. 2011;37(7):903-9.
Hamasha AA, Hatiwsh A. Quality of life and satisfaction of patients after nonsurgical primary root canal treatment provided by undergraduate students, graduate students and endodontic specialists. Int Endod J. 2013;46(12):1131-9.
Dahlström L, Lindwall O, Rystedt H, Reit C. ‘Working in the dark’: Swedish general dental practitioners on the complexity of root canal treatment. Int Endod J. 2017;50(7):636-45.
Sebring D, Dimenas H, Engstrand S, Kvist T. Characteristics of teeth referred to a public dental specialist clinic in endodontics. Int Endod J. 2017;50(7):629-35.
Laukkanen E, Vehkalahti MM, Kotiranta AK. Radiographic outcome of root canal treatment in general dental practice: tooth type and quality of root filling as prognostic factors. Acta Odontol Scand. 2021;79(1):37-42.
Fransson H, Bjørndal L, Frisk F, Dawson VS, Landt K, Isberg PE, et al. Factors Associated with Extraction following Root Canal Filling in Adults. J Dent Res. 2021;100(6):608-14.
Wigsten E, EndoReCo, Kvist T. Patient record assessment of results and related resources spent during 1 year after initiation of root canal treatment in a Swedish public dental organization. Int Endod J. 2022.
Haug SR, Solfjeld AF, Ranheim LE, Bårdsen A. Impact of Case Difficulty on Endodontic Mishaps in an Undergraduate Student Clinic. J Endod. 2018;44(7):1088-95.
Knight A, Blewitt I, Al-Nuaimi N, Watson T, Herzog D, Festy F, et al. Rapid Chairside Microbial Detection Predicts Endodontic Treatment Outcome. J Clin Med. 2020;9(7).
Mente J, Petrovic J, Gehrig H, Rampf S, Michel A, Schurz A, et al. A Prospective Clinical Pilot Study on the Level of Matrix Metalloproteinase-9 in Dental Pulpal Blood as a Marker for the State of Inflammation in the Pulp Tissue. J Endod. 2016;42(2):190-7.
Rechenberg DK, Galicia JC, Peters OA. Biological Markers for Pulpal Inflammation: A Systematic Review. PLoS One. 2016;11(11):e0167289.
Zehnder M, Belibasakis GN. A critical analysis of research methods to study clinical molecular biomarkers in Endodontic research. Int Endod J. 2021.
Patel S, Brown J, Semper M, Abella F, Mannocci F. European Society of Endodontology position statement: Use of cone beam computed tomography in Endodontics: European Society of Endodontology (ESE) developed by. Int Endod J. 2019;52(12):1675-8.
Hol C, Hellen-Halme K, Torgersen G, Nilsson M, Moystad A. How do dentists use CBCT in dental clinics? A Norwegian nationwide survey. Acta Odontol Scand. 2015;73(3):195-201.
Strindberg JE, Hol C, Torgersen G, Moystad A, Nilsson M, Nasstrom K, et al. Comparison of Swedish and Norwegian Use of Cone-Beam Computed Tomography: a Questionnaire Study. J Oral Maxillofac Res. 2015;6(4):e2.
Schwendicke F, Samek W, Krois J. Artificial Intelligence in Dentistry: Chances and Challenges. J Dent Res. 2020;99(7):769-74.
Aminoshariae A, Kulild J, Nagendrababu V. Artificial Intelligence in Endodontics: Current Applications and Future Directions. J Endod. 2021;47(9):1352-7.
Clark D, Khademi J. Modern molar endodontic access and directed dentin conservation. Dent Clin North Am. 2010;54(2):249-73.
Silva E, Pinto KP, Ferreira CM, Belladonna FG, De-Deus G, Dummer PMH, et al. Current status on minimal access cavity preparations: a critical analysis and a proposal for a universal nomenclature. Int Endod J. 2020;53(12):1618-35.
Zehnder MS, Connert T, Weiger R, Krastl G, Kuhl S. Guided endodontics: accuracy of a novel method for guided access cavity preparation and root canal location. Int Endod J. 2016;49(10):966-72.
European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J. 2006 Dec;39(12):921-30.
Markvart M, Fransson H, EndoReCo, Bjorndal L. Ten-year follow-up on adoption of endodontic technology and clinical guidelines amongst Danish general dental practitioners. Acta Odontol Scand. 2018;76(7):515-9.
Leinonen S, Vehkalahti MM. Compliance with Key Practices of Root Canal Treatment Varies by the Reward System Applied in Public Dental Services. J Endod. 2021;47(10):1592-7.
Malmberg L, Hågg E, Björkner AE. Endodontic infection control routines among general dental practitioners in Sweden and Norway: a questionnaire survey. Acta Odontol Scand. 2019;77(6):434-8.
Bergenholtz G. Assessment of treatment failure in endodontic therapy. J Oral Rehabil. 2016;43(10):753-8.
Ruksakiet K, Hanák L, Farkas N, Hegyi P, Sadaeng W, Czumbel LM, et al. Antimicrobial Efficacy of Chlorhexidine and Sodium Hypochlorite in Root Canal Disinfection: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Journal of Endodontics. 2020;46(8):1032-41.e7.
Haapasalo M, Wang Z, Shen Y, Curtis A, Patel P, Khakpour M. Tissue dissolution by a novel multisonic ultracleaning system and sodium hypochlorite. J Endod. 2014;40(8):1178-81.
Sigurdsson A, Garland RW, Le KT, Woo SM. 12-month Healing Rates after Endodontic Therapy Using the Novel GentleWave System: A Prospective Multicenter Clinical Study. J Endod. 2016;42(7):1040-8.
Basrani B, Haapasalo M. Update on endodontic irrigating solutions. Endodontic Topics. 2012;27(1):74-102.
Nair PN, Henry S, Cano V, Vera J. Microbial status of apical root canal system of human mandibular first molars with primary apical periodontitis after “one-visit” endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99(2):231-52.
Ma J, Tong Z, Ling J, Liu H, Wei X. The effects of sodium hypochlorite and chlorhexidine irrigants on the antibacterial activities of alkaline media against Enterococcus faecalis. Arch Oral Biol. 2015;60(7):1075-81.
Kvist T, Molander A, Dahlen G, Reit C. Microbiological evaluation of one- and two-visit endodontic treatment of teeth with apical periodontitis: a randomized, clinical trial. J Endod. 2004;30(8):572-6.
Kumar G, Tewari S, Tagg J, Chikindas ML, Popov IV, Tiwari SK. Can Probiotics Emerge as Effective Therapeutic Agents in Apical Periodontitis? A Review. Probiotics Antimicrob Proteins. 2021;13(2):299-314.
Poveda Roda R, Bagán JV, Sanchis Bielsa JM, Carbonell Pastor EJMO, Patología Oral y Cirugía Bucal. Antibiotic use in dental practice: A review. 2007;12(3):186-92.
Laxminarayan R, Duse A, Wattal C, Zaidi AKM, Wertheim HFL, Sumpradit N, et al. Antibiotic resistance—the need for global solutions. The Lancet Infectious Diseases. 2013;13(12):1057-98.
Laxminarayan R, Heymann DL. Challenges of drug resistance in the developing world. BMJ. 2012;344:e1567.
Prieto-Prieto J, Calvo A. Microbiological basis of oral infections and sensitivity to antibiotics. Med Oral Patol Oral Cir Bucal. 2004;9 Suppl:15-8; 1-4.
Bresco-Salinas M, Costa-Riu N, Berini-Aytes L, Gay-Escoda C. Antibiotic susceptibility of the bacteria causing odontogenic infections. Med Oral Patol Oral Cir Bucal. 2006;11(1):E70-5.
Li G-H, Niu L-N, Zhang W, Olsen M, De-Deus G, Eid AA, et al. Ability of new obturation materials to improve the seal of the root canal system: a review. Acta Biomater. 2014;10(3):1050-63.
Ørstavik D. Endodontic filling materials. Endodontic Topics. 2014;31(1):53-67.
Kim SG, Malek M, Sigurdsson A, Lin LM, Kahler B. Regenerative endodontics: a comprehensive review. Int Endod J. 2018;51(12):1367-88.
Liu Y, Gan L, Cui DX, Yu SH, Pan Y, Zheng LW, et al. Epigenetic regulation of dental pulp stem cells and its potential in regenerative endodontics. World J Stem Cells. 2021;13(11):1647-66.
Lin LM, Huang GT, Sigurdsson A, Kahler B. Clinical cell-based versus cell-free regenerative endodontics: clarification of concept and term. Int Endod J. 2021;54(6):887-901.
Kearney M, Cooper PR, Smith AJ, Duncan HF. Epigenetic Approaches to the Treatment of Dental Pulp Inflammation and Repair: Opportunities and Obstacles. Front Genet. 2018;9:311.
Baaij A, Ozok AR, Vth M, Musaeus P, Kirkevang LL. Self-efficacy of undergraduate dental students in Endodontics within Aarhus and Amsterdam. Int Endod J. 2020;53(2):276-84.
Haug SR, Linde BR, Christensen HQ, Vilhjalmsson VH, Bårdsen A. An investigation into security, self-confidence and gender differences related to undergraduate education in Endodontics. Int Endod J. 2021;54(5):802-11.
Gatley S, Hayes J, Davies C. Requirements, in terms of root canal treatment, of undergraduates in the European Union: an audit of teaching practice. Br Dent J. 2009;207(4):165-70.
Qualtrough AJ. Undergraduate endodontic education: what are the challenges? Br Dent J. 2014;216(6):361-4.
Patel J, Fox K, Grieveson B, Youngson CC. Undergraduate training as preparation for vocational training in England: a survey of vocational dental practitioners’ and their trainers’ views. British dental journal. 2006;201(S5):9-15.
Whitney EM, Walton JN, Aleksejuniene J, Schönwetter DJ. Graduating Dental Students’ Views of Competency Statements: Importance, Confidence, and Time Trends from 2008 to 2012. J Dent Educ. 2015;79(3):322-30.
Christensen HQ, Linde BR, Bårdsen A, Vilhjalmsson VH, Haug SR. Influence of dental education on adoption and integration of technological aids in the delivery of endodontic care by dental practitioners: a survey. Acta Odontologica Scandinavica. 2022:1-8.
Tsesis I, Rosen E, Taschieri S, Telishevsky Strauss Y, Ceresoli V, Del Fabbro M. Outcomes of Surgical Endodontic Treatment Performed by a Modern Technique: An Updated Meta-analysis of the Literature. Journal of Endodontics. 2013;39(3):332-9.
D’Souza RN, Colombo JS. How Research Training Will Shape the Future of Dental, Oral, and Craniofacial Research. Chicago2017. p. eS73-eS82.
Wigsten E, Jonasson P, EndoReCo, Kvist T. Indications for root canal treatment in a Swedish county dental service: patient- and tooth-specific characteristics. Int Endod J. 2019;52(2):158-68.
Wigsten E, Al Hajj A, Jonasson P, EndoReCo, Kvist T. Patient satisfaction with root canal treatment and outcomes in the Swedish public dental health service. A prospective cohort study. Int Endod J. 2021.
Zilinskaite-Petrauskiene I, Haug SR. A Comparison of Endodontic Treatment Factors, Operator Difficulties, and Perceived Oral Health–related Quality of Life between Elderly and Young Patients. Journal of Endodontics. 2021;47(12):1844-53.
Bletsa A, Iden O, Sulo G, Berggreen E. Work experience influences treatment approaches in endodontics: a questionnaire survey among dentists in Western Norway. Acta Odontol Scand. 2019;77(8):617-23.
Hull EE, Montgomery MR, Leyva KJ. HDAC Inhibitors as Epigenetic Regulators of the Immune System: Impacts on Cancer Therapy and Inflammatory Diseases. Biomed Res Int. 2016;2016:8797206.
Duncan HF, Smith AJ, Fleming GJ, Cooper PR. Histone deacetylase inhibitors induced differentiation and accelerated mineralization of pulp-derived cells. J Endod. 2012;38(3):339-45.
Corresponding author: Anca Virtej. E-mail: Anca.Virtej@uib.no
Accepted for publication 06.08.2022
The article is peer reviewed.
Virtej A, Wigsten E, Ørstavik D, Haug SR. Future directions in endodontics. Nor Tannlegeforen Tid. 2023; 133:
Keywords: Dental education; Health Authorities; Innovations; Quality of life; Research
